Understanding Pulmonary Embolism
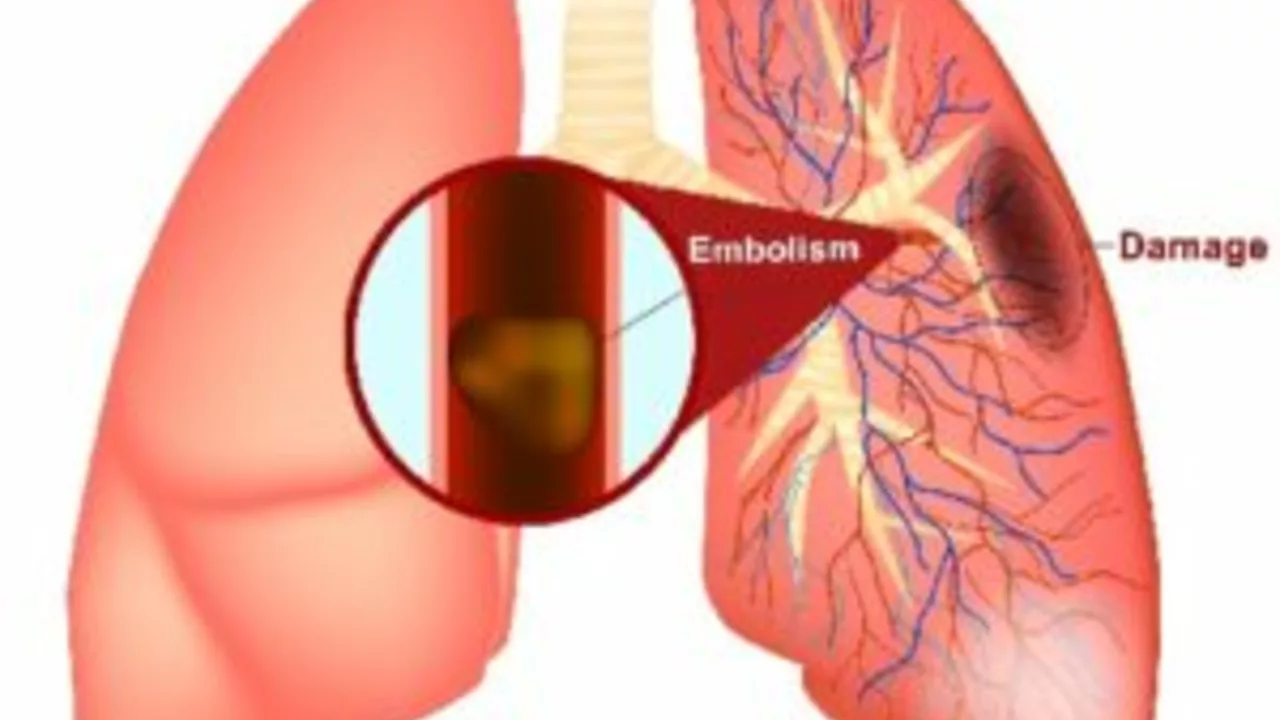
I remember that rainy day when a close friend of mine was diagnosed with a condition known as Pulmonary Embolism, or PE for short. I was surprised, to say the least. It felt like a scene straight out of a medical drama, only this time, the drama was real and it involved someone close to me. What’s PE, you ask? Simply put, Pulmonary Embolism is when one or more of the arteries in your lungs gets blocked by a blood clot. It's a serious condition that can result in significant health complications or even death if not treated properly.
But what was more daunting was that I didn't know how to support them. I was adrift in a sea of medical jargon and frightful prognoses. Well, dear readers, I’ve learned a thing or two since then. Allow me, Nathaniel, to share my observations and experiences about supporting a loved one diagnosed with PE. But before that, let's dive deep into understanding this medical condition better.
Debunking Pulmonary Embolism Myths
There’s a lot of scary sounding information flying around on the internet about PE. Trust me, I've read through most of it. It’s overwhelming and a good chunk of it is just not true. So, let me help you filter some of that noise. The first thing you need to know is that not all blood clots lead to PE. I repeat - not all blood clots lead to PE. PE is only caused when a blood clot in another part of your body, usually your leg, breaks away and travels up to your lungs.
Here's a fun fact, did you know that even long aeroplane flights can increase the risk of PE? It is not entirely understood why, but the prolonged immobility could play a role in this, as it slows down circulation and makes it more likely for blood clots to form. This is called "economy class syndrome," although it does not only affect those in economy class!
Navigating the Medical Maze
Supporting a loved one with PE is not just about emotional support; it also involves helping them work through the maze of medical appointments and medication schedules, all while understanding the probability of a reoccurrence. In simple terms, once a PE happens, there's an increased chance of it happening again. Reducing this chance is where the treatment comes in. Typical treatment involves blood thinners supplied in entire textbook names like Warfarin or Dabigatran. See, even I had to practice a few times before I could pronounce it right.
Something that took me by surprise was the sheer number of follow-up appointments and blood tests my friend needed following the diagnosis. I was the calendar keeper, remembering doctor's visits and keeping track of medication. In the process, I discovered I have a knack for organisation.
Offering Emotional Support
While doctors can be very competent at treating the physical symptoms of PE, they unfortunately do not come with an in-built emotion processor to deal with the many feelings a patient might experience. That's where you come in. Be there for your loved ones, offer them a shoulder to lean on, a listening ear, a hand to hold. Let them know they are not alone in their journey.
In my friend's case, it was oddly therapeutic to sit and listen to him express his fears, anxieties, and hopes too. The importance of empathetic listening cannot be overstated here. It helps to remind them that they are more than just their diagnosis, an emotional crutch, if you will. And remember, it's okay to laugh and have fun. Encourage them to pursue hobbies or interests that may help keep spirits high. Who knows? You may end up discovering shared interests! That's how my friend and I ended up going through a Monty Python marathon.
Healthy Living Tips for Pulmonary Embolism
I am no doctor, but I sure have picked up few tips that can help one live a healthier life post a PE diagnosis. Sticking to the medication plan, regular walks, balanced meals and no smoking are typically top of the list, not to mention the importance of hydration. It may sound like stating the obvious, but these simple steps can significantly improve the quality of life and reduce the risk of a second PE.
PE should be treated with the seriousness it deserves, but it doesn't have to be a black cloud hanging over one's existence. My friend, for instance, joined a gym following his doctor's advice and discovered his love for yoga. Apparently, it not only helped with the circulation (which is good for preventing clots) but also gave him an excuse to stock up on comfortable yoga pants. Now, I’m considering joining him for the stylish wardrobe alone.
In conclusion, remember, supporting a loved one with PE is a journey, not a sprint. It may get frustrating and tiring at times, but the reward of seeing your loved one get better, that's worth everything. As for me? I have learned a great deal from this journey. And much like a good cup of tea on a cold London day, it's these little things in life that make it worthwhile.

Dhakad rahul
Yo, I read this whole saga on PE and felt like I was watching a Bollywood blockbuster-full of drama, twists, and those over‑the‑top hero moments! 😎💥 It's crazy how a tiny clot can turn someone's life into an epic tragedy, and yet we all act like it’s just another episode of a medical drama series. 🙄 But seriously, if you’re the sidekick, you gotta be the one who keeps the script in order-appointments, meds, the whole nine yards. 🎬 And don’t even get me started on the “economy class syndrome” myth-people act like it's some government conspiracy to keep us grounded. 🛫🛑 The truth? Move around, stretch, and maybe don’t binge‑watch series for 12 hours straight. 🎮💤 Anyway, stay strong, stay organized, and remember: you’re not a background extra, you’re the lead in this story! 💪🏽🇮🇳