Understanding Idiopathic Pulmonary Fibrosis
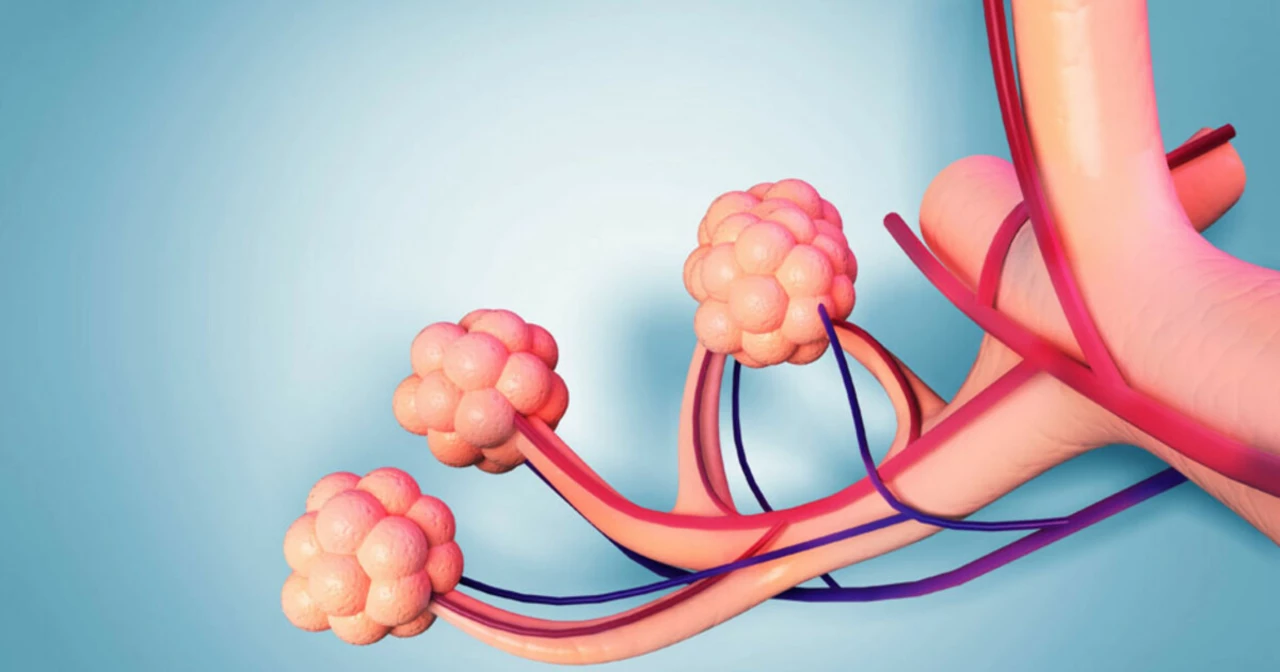
As an individual in the healthcare field, I often come across various health conditions that affect countless lives. One such condition is Idiopathic Pulmonary Fibrosis (IPF), a progressive lung disease that causes the tissue in the lungs to become thick and scarred, making it difficult for the individual to breathe. The term "idiopathic" refers to the fact that the cause of this disease is still unknown. In this section, I will provide an overview of what IPF is, its symptoms, and the risk factors associated with it.
IPF primarily affects older adults and is characterized by a decline in lung function over time. Symptoms of IPF include shortness of breath, chronic dry cough, fatigue, and unexplained weight loss. Some of the risk factors for developing IPF include smoking, exposure to certain environmental factors, and a family history of the disease. Unfortunately, there is no cure for IPF, and the progression of the disease varies from person to person. With that said, let's dive into the future of IPF research and treatment to understand what is being done to combat this debilitating disease.
Current Treatment Options for IPF
As a blogger, I have seen a gradual increase in the number of treatment options available for IPF patients. Currently, there are two FDA-approved medications, pirfenidone and nintedanib, which have been shown to slow the progression of the disease. However, these drugs are not a cure and only help to manage the symptoms. In addition to medication, other treatment options include supplemental oxygen therapy, pulmonary rehabilitation, and lung transplantation in severe cases.
Although these treatment options can improve the quality of life for some patients, there is still a long way to go in terms of finding a cure for IPF. The availability of new and effective treatments is crucial in managing this devastating disease. This brings us to the next section, where we will discuss the ongoing research in the field of IPF and its implications for the future of treatment.
Advancements in IPF Research
Research in the field of IPF has come a long way in recent years, with scientists working tirelessly to understand the underlying causes of the disease and develop new treatment options. One of the most promising areas of research is the identification of genetic factors that may contribute to the development of IPF. This could potentially pave the way for the development of personalized medicine, allowing doctors to tailor treatment plans based on an individual's genetic makeup.
Another exciting area of research is the study of the role of cellular aging in IPF. Recent studies have shown that the cells in the lungs of IPF patients age more rapidly than those in healthy individuals. This has led to the development of drugs that target the aging process, with the hope that they may slow the progression of the disease. In the following sections, we will explore these and other advancements in IPF research in greater detail.
Exploring the Role of Genetics in IPF
As I mentioned earlier, one of the most promising areas of IPF research is the study of genetics. Researchers have identified several genes that are associated with an increased risk of developing IPF. Some of these genes play a role in the body's immune response, while others are involved in the production of collagen, a protein that provides structure to the lungs. By understanding how these genes contribute to the development of IPF, scientists hope to develop targeted therapies that can prevent or slow the progression of the disease.
Moreover, the identification of these genetic risk factors has also led to the discovery of potential biomarkers for IPF. Biomarkers are measurable indicators of a biological process and can be used to diagnose or monitor the progression of a disease. In the case of IPF, these biomarkers could be used to identify individuals at risk for the disease before symptoms develop, allowing for earlier intervention and treatment.
Targeting Cellular Aging in IPF
The study of cellular aging in IPF is another fascinating area of research that I have been following closely. As I mentioned earlier, recent studies have shown that the cells in the lungs of IPF patients age more rapidly than those in healthy individuals. This accelerated aging process, known as senescence, is believed to contribute to the development of fibrosis, or scarring, in the lungs.
Researchers are now exploring ways to target senescence in order to slow the progression of IPF. One such approach involves the use of drugs called senolytics, which selectively eliminate senescent cells from the body. By removing these aged cells, researchers hope to reduce inflammation and fibrosis in the lungs, ultimately improving lung function and quality of life for IPF patients.
The Future of Personalized Medicine in IPF
The advancements in genetics and cellular aging research have laid the groundwork for the development of personalized medicine in IPF. Personalized medicine refers to the customization of healthcare based on an individual's unique genetic makeup, lifestyle, and environmental factors. By understanding how these factors contribute to the development and progression of IPF, doctors will be able to tailor treatment plans to each patient's specific needs.
For example, genetic testing could be used to identify individuals who are at a higher risk of developing IPF. These individuals could then be monitored more closely and potentially receive early intervention to slow the progression of the disease. Additionally, the development of targeted therapies based on a patient's genetic profile could lead to more effective treatments with fewer side effects.
Collaboration and Funding in IPF Research
As a blogger, I am always inspired by the collaborative efforts and funding sources that drive research in the field of IPF. Several organizations, including the Pulmonary Fibrosis Foundation and the National Institutes of Health, provide funding and support for IPF research. Additionally, organizations such as the American Thoracic Society and the European Respiratory Society bring together researchers from around the world to share their findings and collaborate on new projects.
This collaborative approach has led to significant breakthroughs in our understanding of IPF and the development of new therapies. As research continues to advance, I am hopeful that we will see even more progress in the field of IPF, ultimately leading to better treatment options and, one day, a cure for this devastating disease.
Conclusion: A Hopeful Future for IPF Patients
As I conclude this article, I am filled with a sense of hope and optimism for the future of IPF research and treatment. The advancements in genetics, cellular aging research, and personalized medicine have the potential to revolutionize the way we diagnose and treat IPF. With continued collaboration and funding, I believe that we are on the cusp of discovering new therapies that can significantly improve the quality of life for IPF patients.
As a blogger, I will continue to follow the latest developments in IPF research and share them with you, my readers. Together, we can raise awareness of this disease and support the ongoing efforts to find a cure. In the meantime, I encourage you to educate yourself about IPF, support research initiatives, and advocate for those living with this challenging disease.

Marcus Edström
I really appreciate the comprehensive overview on IPF.
It's great to see both the clinical perspective and the research outlook in one place.
The way you broke down the genetics and cellular aging sections made it easy to follow.
Collaboration between pulmonologists and geneticists seems crucial moving forward.
Looking forward to more updates as the field evolves.