Understanding Amenorrhea and Its Effects on Women
Amenorrhea is defined as the absence of menstruation in a woman of reproductive age. This condition can be caused by various factors, ranging from hormonal imbalances to lifestyle choices. In this article, we will discuss the link between amenorrhea and osteoporosis, a condition characterized by weak and brittle bones. We will explore the reasons behind this connection and offer valuable insights into how to prevent and manage both conditions effectively.
The Hormonal Connection: Estrogen and Bone Health
Estrogen is a hormone that plays a crucial role in maintaining bone strength and density in women. It helps regulate the process of bone remodeling, which involves the removal of old bone tissue and the formation of new bone. When a woman experiences amenorrhea, her body may not produce enough estrogen, leading to an imbalance in the bone remodeling process.
As a result, the rate of bone loss may exceed the rate of new bone formation, eventually leading to osteoporosis. This is particularly concerning for young women who have not yet reached their peak bone mass. The longer a woman experiences amenorrhea, the greater her risk of developing osteoporosis later in life.
Identifying the Causes of Amenorrhea
Amenorrhea can be classified into two types: primary and secondary. Primary amenorrhea occurs when a girl has not started menstruating by the age of 16. This can be caused by structural abnormalities, hormonal imbalances, or genetic factors. Secondary amenorrhea occurs when a woman who has previously menstruated stops having periods for at least three months. This is more commonly associated with the development of osteoporosis.
Some of the potential causes of secondary amenorrhea include polycystic ovary syndrome (PCOS), thyroid disorders, extreme weight loss, excessive exercise, and stress. Identifying and addressing the underlying cause of amenorrhea is crucial in preventing the development of osteoporosis and other health issues.
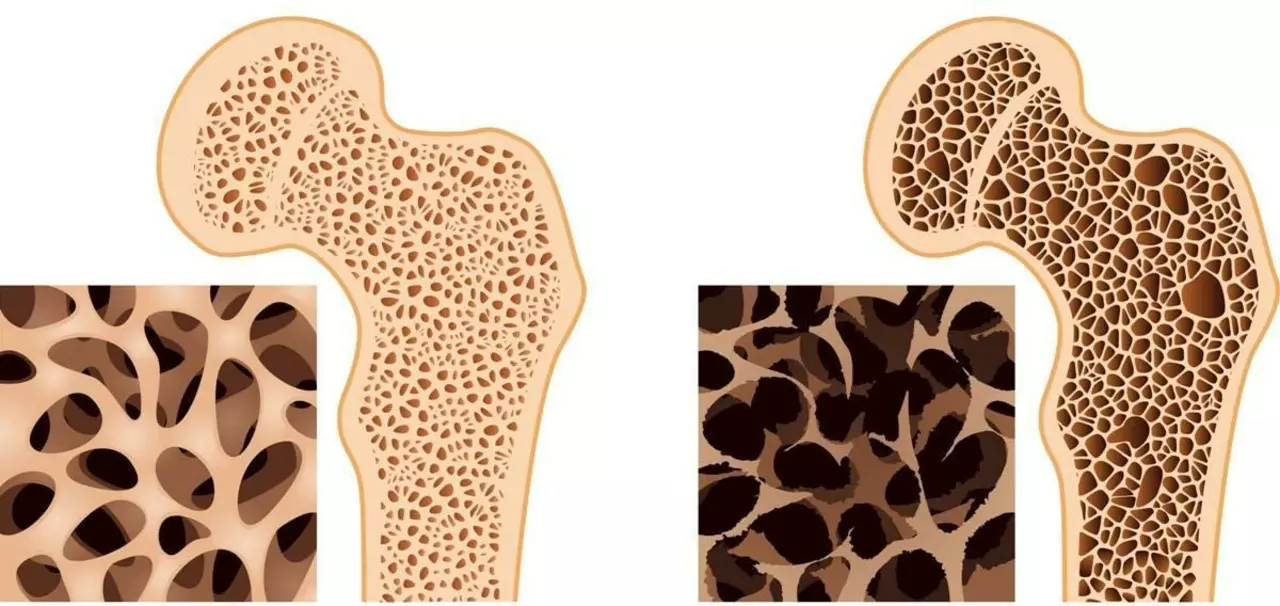
Recognizing the Symptoms of Osteoporosis
Osteoporosis is often called a "silent disease" because it typically does not cause noticeable symptoms until a fracture occurs. However, some warning signs may indicate that a woman's bone density is decreasing. These can include back pain, loss of height, stooped posture, and frequent bone fractures.
If you have amenorrhea and any of these symptoms, it is essential to consult a healthcare professional. They can perform a bone density test to determine your risk of developing osteoporosis and recommend appropriate interventions if necessary.
Preventing Osteoporosis through Nutrition and Exercise
A balanced diet and regular exercise are essential components of a healthy lifestyle, and they play a significant role in maintaining bone health. Consuming adequate amounts of calcium and vitamin D is crucial for building and maintaining strong bones. Good sources of calcium include dairy products, leafy green vegetables, and fortified foods. Vitamin D can be obtained through sunlight exposure, certain foods like fatty fish, and supplements.
Weight-bearing exercises, such as walking, jogging, dancing, and resistance training, can help stimulate bone growth and slow down bone loss. Aim for at least 30 minutes of weight-bearing exercise most days of the week, along with strength training exercises that target all major muscle groups at least twice a week.
Addressing Amenorrhea through Lifestyle Modifications
Depending on the cause of amenorrhea, certain lifestyle changes may help restore regular menstruation and improve bone health. For women with amenorrhea due to excessive exercise or extreme weight loss, decreasing the intensity of workouts and achieving a healthy body weight may help regulate periods.
Managing stress through relaxation techniques, such as yoga, meditation, or deep breathing exercises, can also be beneficial for women experiencing amenorrhea due to high stress levels. If a hormonal imbalance, such as PCOS or a thyroid disorder, is the cause of amenorrhea, medical treatment may be necessary to regulate periods and maintain bone health.
Medical Treatment Options for Amenorrhea and Osteoporosis
When lifestyle changes are not sufficient to address amenorrhea and the associated risk of osteoporosis, medical treatment may be necessary. Hormonal therapies, such as oral contraceptives or hormone replacement therapy, can help restore regular menstruation and improve bone health in some women.
For women who have already developed osteoporosis, medications like bisphosphonates, denosumab, or teriparatide can help slow down bone loss and reduce the risk of fractures. It is essential to work closely with a healthcare professional to determine the most appropriate treatment plan for your specific situation.
The Importance of Early Detection and Intervention
Understanding the link between amenorrhea and osteoporosis is crucial for women's health. Early detection of both conditions and timely intervention can help prevent long-term complications and improve overall well-being.
If you have concerns about your menstrual cycle or bone health, consult your healthcare provider for a thorough evaluation and guidance on appropriate preventive measures or treatment options. By addressing the underlying cause of amenorrhea and promoting bone health, you can reduce your risk of developing osteoporosis and enjoy a healthier, more active life.

Elle Trent
Wow, this piece is basically a textbook on estrogen‑centric bone remodeling, drenched in medical jargon that would make a PhD sigh. The link between amenorrhea and osteoporosis is presented like a Hollywood drama, complete with the “silent disease” cliché. Honestly, a layperson might get lost in the sea of terms like "bone density test" and "weight‑bearing exercise" without clear take‑aways. A more concise, plain‑English summary would do wonders for readers actually trying to protect their bones.