Drug Interaction Checker
Check Medication Interactions
Enter up to 3 medications to see potential interactions and their risks
Potential Interaction Found
When you take more than one medication, something invisible is happening inside your body. Two drugs might be fighting over the same space, blocking each other’s path, or even teaming up to create a dangerous effect. These are drug-drug interactions - and they’re more common than most people realize. In fact, about 1 in 20 hospital admissions for older adults is linked to a preventable interaction between medications. This isn’t about side effects from a single drug. It’s about what happens when drugs collide.
How Drugs Talk to Each Other: The Two Main Ways
Not all drug interactions are the same. They fall into two clear categories: pharmacokinetic and pharmacodynamic. One is about how much of a drug gets to your bloodstream. The other is about what the drug does once it’s there.
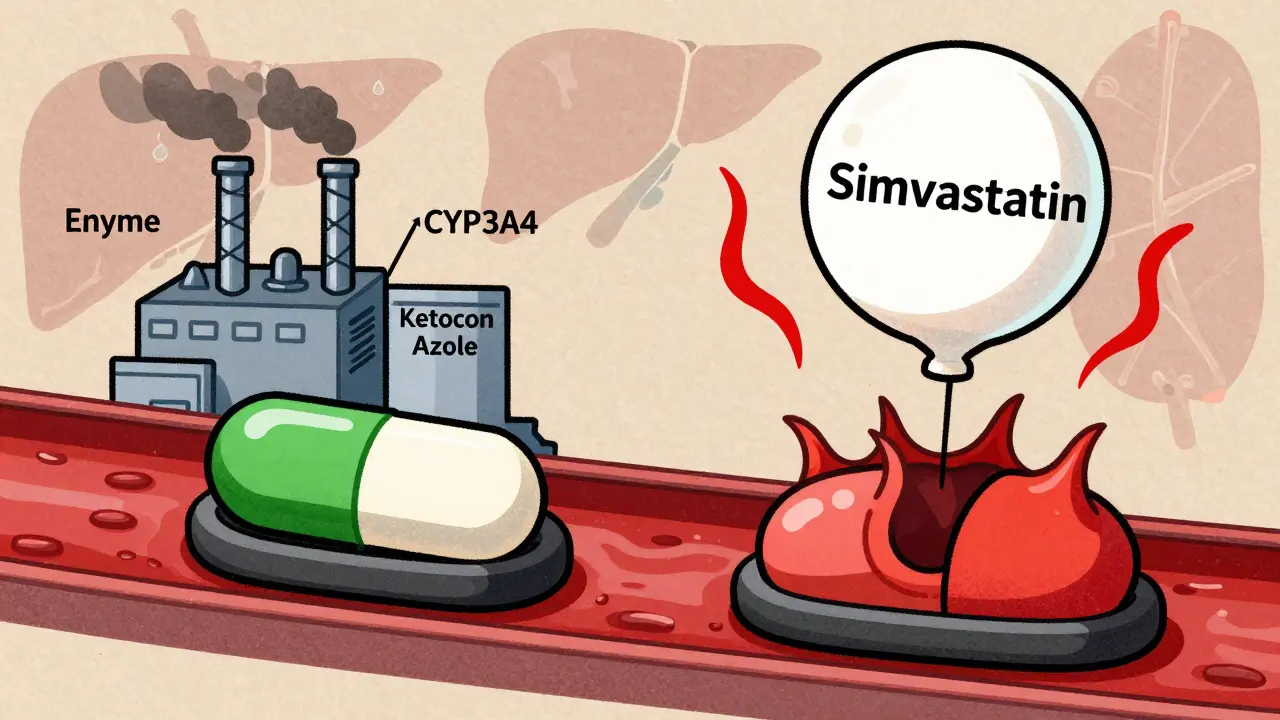
Pharmacokinetic interactions change how your body handles a drug. Think of it like traffic control. One drug might slow down the absorption of another in your gut, block it from being broken down by liver enzymes, or stop your kidneys from flushing it out. The result? Too much or too little of the drug in your system. For example, if you take ketoconazole (an antifungal) with simvastatin (a cholesterol drug), ketoconazole shuts down the liver enzyme CYP3A4 that normally breaks down simvastatin. Simvastatin levels can spike 10 to 20 times higher than normal. That’s not just a tweak - it’s a red alert for muscle damage called rhabdomyolysis.
Pharmacodynamic interactions are about what happens when two drugs meet at their target. They don’t change each other’s levels. Instead, they change each other’s effects. Imagine one drug turns up the volume on a signal, and another turns it down. Or worse - both turn it up together. Take fluoroquinolone antibiotics and macrolides like erythromycin. Alone, each can slightly prolong the heart’s QT interval. Together, they multiply the risk by over five times, triggering a dangerous heart rhythm called torsades de pointes. Or consider ACE inhibitors (like lisinopril) and potassium-sparing diuretics (like amiloride). Both raise potassium levels. Together, they can push potassium into the danger zone, risking cardiac arrest.
The Big Players: CYP Enzymes and Transporters
Most pharmacokinetic interactions happen because of two key systems: the cytochrome P450 enzymes and drug transporters.
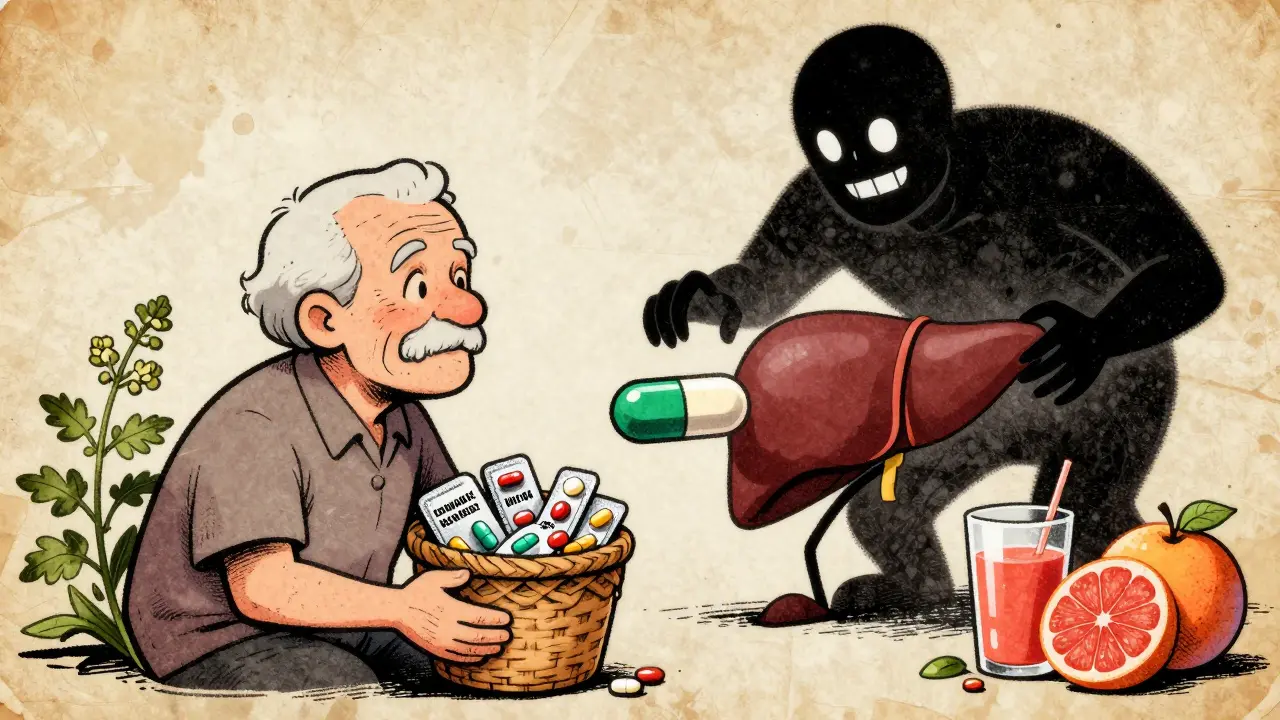
The CYP system - especially CYP3A4, CYP2D6, CYP2C9, and CYP2C19 - handles about 70 to 80% of all drug metabolism. CYP3A4 alone breaks down half of all prescription drugs. When something blocks this enzyme (an inhibitor), drugs build up. When something boosts it (an inducer), drugs vanish too fast. St. John’s Wort, a popular herbal supplement, is a powerful CYP3A4 inducer. It can slash the blood levels of cyclosporine (used after organ transplants) by 50 to 60%, risking organ rejection. That’s not a myth - it’s a documented, life-threatening interaction.
Transporters are like bouncers at a club. They decide which drugs get into or out of cells. P-glycoprotein (P-gp) is one of the most important. It pushes drugs out of brain cells, kidney cells, and intestinal cells. When verapamil (a heart medication) blocks P-gp, digoxin (another heart drug) floods into the bloodstream. Levels can jump 50 to 100%. That’s enough to cause deadly arrhythmias. These aren’t rare edge cases. They’re routine risks for millions.
Who’s the Perpetrator? Who’s the Victim?
In drug interaction lingo, one drug is the perpetrator - the one causing the change. The other is the victim - the one being affected. A drug can be both. Verapamil, for example, is a perpetrator when it blocks CYP3A4 or P-gp. But it’s also a victim - because CYP3A4 breaks it down. So if you take a CYP3A4 inducer like rifampin with verapamil, your verapamil levels crash. Your blood pressure control fails. This bidirectional dance is why interactions are so hard to predict.
Perpetrators are ranked by strength: strong, moderate, or weak. A strong inhibitor like clarithromycin can raise a victim drug’s concentration by over five times. A weak one might only nudge it up by 20%. The FDA and EMA use this scale to guide warnings. If a drug is a strong CYP3A4 inhibitor, the label will say: “Avoid with simvastatin.” No gray area.
Why Some People Are at Higher Risk
Not everyone reacts the same way. Genetics play a huge role. About 5% of people have a CYP2D6 gene variant that makes them “poor metabolizers.” They break down drugs like codeine, tramadol, or antidepressants much slower. If they take a CYP2D6 inhibitor like fluoxetine on top of that, codeine can’t turn into morphine - so it doesn’t work. But if they’re an “ultrarapid metabolizer,” codeine turns into morphine too fast. Add a CYP3A4 inhibitor, and the morphine level spikes. That’s how someone can overdose on codeine without taking more than prescribed.
Age matters too. As we get older, liver and kidney function decline. Drugs stick around longer. Elderly patients often take five or more medications - the perfect storm for interactions. The Beers Criteria, updated in 2019, lists 30 high-risk combinations for older adults. One of the top ones? NSAIDs (like ibuprofen) with blood thinners like warfarin. Together, they triple or quadruple the risk of bleeding. That’s why many doctors now avoid NSAIDs entirely in patients on anticoagulants.
Real-World Impact: Hospitals, Costs, and Deaths
This isn’t theoretical. The FDA’s adverse event database tracked over 12,000 reports linked to drug interactions between 2010 and 2020. Warfarin showed up in nearly 30% of them. Antidepressants in 15%. And it’s not just about emergencies. A 2019 study found preventable drug interactions cost the U.S. healthcare system $1.3 billion a year - mostly from hospital stays for bleeding or muscle damage.
Pharmacists are on the front lines. A 2021 study showed pharmacist-led reviews cut serious interactions by 37% in over 12,000 patients. They catch what doctors miss. They ask: “Are you taking St. John’s Wort?” “Do you use OTC painkillers daily?” These questions save lives.
Technology Can Help - But It’s Flawed
Hospitals and clinics use electronic health records with built-in drug interaction alerts. Sounds smart, right? But here’s the catch: 80 to 90% of those alerts are false alarms. A nurse sees 50 alerts in a shift. 45 of them are irrelevant. After a while, they just click “ignore.” This is called alert fatigue. A 2022 study found clinicians override 49 to 96% of alerts. That’s not user error - it’s bad design.
Newer systems are smarter. Epic’s “Suggestive Warnings,” launched in 2021, only pops up when the interaction is severe and the patient is actually taking both drugs. In one trial, it cut high-severity interactions by 22%. That’s progress.
The Future: Personalized Medicine and AI
The next big leap is personalization. The Clinical Pharmacogenetics Implementation Consortium (CPIC) now has 22 guidelines that tie genetics to drug interactions. For example: if you’re a CYP2D6 ultrarapid metabolizer, avoid codeine - especially if you’re also taking a CYP3A4 inhibitor. This isn’t science fiction. It’s standard practice in some hospitals.
Artificial intelligence is catching up too. A 2021 study trained a machine learning model on 89 million electronic health records. It predicted dangerous interactions with 94.8% accuracy - far better than old rule-based systems. These tools don’t just flag interactions. They rank risk, suggest alternatives, and even predict how long an interaction will last.
What You Can Do
You don’t need a PhD to protect yourself. Here’s how:
- Keep a full list of everything you take - prescriptions, OTC meds, supplements, herbs. Include doses and how often you take them.
- Ask your pharmacist every time you get a new prescription: “Could this interact with anything I’m already taking?”
- Never start an herb or supplement without checking. St. John’s Wort, garlic, ginkgo, and grapefruit juice are common offenders.
- Use trusted tools. The Liverpool HIV-Drug Interactions Checker is free and updated daily. Even if you’re not living with HIV, it covers hundreds of drugs.
- Know your high-risk drugs. Warfarin, digoxin, statins, anticonvulsants, and some antidepressants have narrow safety margins. One small interaction can be dangerous.
Drug interactions aren’t accidents. They’re predictable. And with the right knowledge - and a little caution - most of them are avoidable.

Sonja Stoces
I’ve seen so many patients on warfarin + ibuprofen and just… how? 😒 Like, is this really still a thing in 2024? I had one guy come in with a GI bleed and swear he ‘only took it for his arthritis’ like it was a snack. St. John’s Wort? Please. It’s not herbal, it’s a chemical warfare agent in a capsule. 🤦♀️