Asthma isn’t just about wheezing. It’s a complex, lifelong condition where your airways swell, tighten, and flood with mucus-making every breath feel like trying to suck air through a straw. About 300 million people worldwide live with it, and in the UK alone, roughly 5.4 million people are diagnosed. The good news? Most people can manage it well. The key is understanding your type, what sets it off, and how your meds really work-especially the difference between inhalers and oral pills.
What Are the Main Types of Asthma?
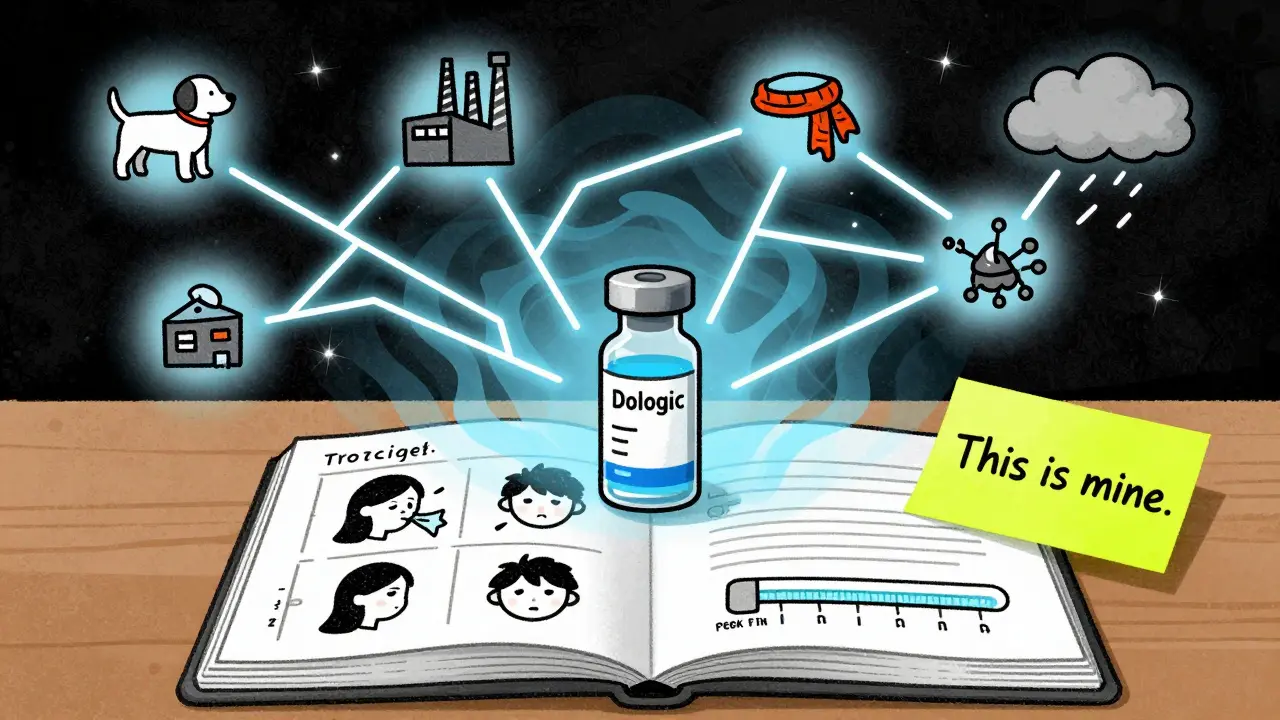
Asthma doesn’t look the same for everyone. It’s broken down by what causes it and how your body reacts. The most common types you’ll hear about:- Allergic asthma-triggered by pollen, dust mites, pet fur, or mold. This is the most common type, especially in kids. If your symptoms spike during hay fever season or after hugging your dog, this is likely you.
- Exercise-induced asthma-symptoms show up during or right after physical activity. You might feel tightness in your chest after running or playing sports, even if you’re otherwise healthy.
- Occupational asthma-caused by workplace irritants like chemical fumes, dust, or gases. Think bakery workers (flour dust), factory staff (isocyanates), or cleaners (strong sprays).
- Cough-variant asthma-you don’t wheeze. You just have a dry, persistent cough that won’t go away. Many people are misdiagnosed with bronchitis for months before realizing it’s asthma.
- Nighttime asthma-symptoms get worse between midnight and 4 a.m. This isn’t just bad luck. Your body’s natural rhythms lower steroid levels at night, and lying down can make mucus pool in your airways.
- Aspirin-induced asthma-a reaction to NSAIDs like ibuprofen or aspirin. If you’ve ever had a breathing attack after taking painkillers, this could be the cause.
- Severe asthma-affects about 4% of asthma patients. Even with high-dose inhalers, symptoms don’t settle. You might need oral steroids just to stay stable.
Doctors now also talk about endotypes-the hidden biology behind your asthma. Eosinophilic asthma means your body produces too many white blood cells called eosinophils that inflame your airways. Neutrophilic asthma involves different cells. Knowing your endotype helps pick the right treatment, especially biologics.
What Triggers Asthma Attacks?
Triggers are the sparks that turn quiet asthma into a full-blown attack. Some are obvious. Others sneak up on you.- Allergens-pollen, dust mites, cockroaches, pet dander. These are the big ones for allergic asthma. Keep your bedroom clean. Use allergen-proof bedding. Wash sheets weekly in hot water.
- Weather-cold, dry air is a major trigger. So is sudden temperature change. In winter, cover your nose and mouth with a scarf when outside.
- Air pollution-smog, car exhaust, smoke from fires. Even secondhand smoke can set off symptoms. Avoid walking on busy roads during rush hour.
- Respiratory infections-colds, flu, even COVID-19. These are the top reason for hospital visits in asthma patients. Get your flu shot every year.
- Stress and strong emotions-laughing too hard, crying, anxiety. These can change your breathing pattern and trigger tightening in the airways.
- Medications-aspirin, ibuprofen, beta-blockers (used for high blood pressure or heart issues). If you’re unsure, check with your doctor before taking anything new.
- Strong smells-perfumes, cleaning products, paint fumes. These don’t cause asthma, but they can make it worse.
One big myth? All triggers affect everyone the same. They don’t. Your triggers are yours alone. Keep a symptom diary for a few weeks. Note what you did, where you were, and what you were exposed to before each episode. You’ll start seeing patterns.
Inhalers: The First Line of Defense
Inhalers are the backbone of asthma care. They deliver medicine straight to your lungs-where it’s needed-without flooding your whole body. That’s why they’re safer and more effective than pills for daily use.There are two main kinds:
- Reliever inhalers (SABAs)-like salbutamol (Ventolin). These work fast-within minutes-to relax tight airways. You use them when you feel symptoms coming on. They’re your emergency tool. But if you’re using one more than twice a week (not counting exercise), your asthma isn’t well controlled.
- Preventer inhalers (ICS)-like fluticasone or budesonide. These reduce swelling and mucus over time. You use them every day, even when you feel fine. They don’t help right away. It takes days or weeks to build up protection.
- Combination inhalers-ICS + LABA (long-acting bronchodilator). These are for moderate to severe asthma. Examples: Seretide (fluticasone/salmeterol), Symbicort (budesonide/formoterol). Some newer ones, like Symbicort, can also act as a reliever in mild cases-this is called SMART therapy.
Here’s the catch: most people use inhalers wrong. A 2023 study found 60-80% of users make at least one critical mistake. Common errors:
- Not shaking the inhaler before use
- Pressing the canister too early or too late
- Not holding your breath after inhaling
- Not using a spacer (especially for kids or during flare-ups)
Spacers are plastic tubes that attach to your inhaler. They hold the medicine so you can breathe it in slowly. Without one, up to 80% of the dose hits your throat and gets swallowed-not your lungs. Ask your nurse or pharmacist to check your technique. It takes five minutes, and it could save your life.
Oral Medications: When Inhalers Aren’t Enough
Oral meds aren’t the go-to. They’re the backup. And they come with serious trade-offs.The most common oral asthma meds:
- Oral corticosteroids (like prednisone)-used for severe flare-ups or when asthma is uncontrolled despite inhalers. They work fast and powerfully. But long-term use? That’s where the damage starts. Side effects include weight gain (68% of users), bone thinning (30-50% higher fracture risk), high blood sugar (5-10% develop diabetes), mood swings, and insomnia. Many patients say they feel like a different person during a steroid course.
- Leukotriene modifiers (like montelukast)-taken as a daily tablet. They block chemicals that cause airway swelling. Used as add-on therapy, especially for allergic or exercise-induced asthma. Side effects are mild-headache, stomach upset. Rarely, they can affect mood. The FDA added a black box warning for depression and suicidal thoughts in 2020.
Experts agree: oral steroids should never be used daily unless absolutely necessary. The Global Initiative for Asthma (GINA) says regular use increases long-term harm more than it helps control symptoms. That’s why doctors push hard to get you off them.
But here’s the reality: for some people with severe asthma, there’s no choice. If you’re on prednisone twice a year or more, or you’ve been hospitalized for asthma, you’re in the severe category. That’s when biologics come in.
Biologics: The New Frontier
Biologics are injectable or IV drugs that target specific parts of your immune system. They’re not for everyone. Only for severe asthma with a clear biological marker-usually high eosinophils.Examples:
- Mepolizumab (Nucala)-targets IL-5, a protein that makes eosinophils. Reduces attacks by 50-60% in trials.
- Tezepelumab (Tezspire)-works even if you don’t have high eosinophils. A breakthrough for non-allergic severe asthma.
These aren’t cheap. A single injection can cost over £1,000. But in the UK, they’re available on the NHS for qualifying patients. Most users report big improvements: fewer hospital visits, less need for steroids, better sleep, more energy. On patient forums, 82% say they’d never go back to daily prednisone.
Why Inhalers Win Over Pills-Most of the Time
Let’s cut through the noise. Inhalers are better for almost everyone. Here’s why:- Targeted delivery-meds go straight to lungs. Less side effects.
- Lower cost long-term-generic inhalers cost £10-£30/month. Oral steroids? You might need them for weeks at a time, and they cause expensive complications like osteoporosis or diabetes.
- More control-you can adjust use based on symptoms. Pills are all-or-nothing.
- Less stigma-nobody notices you using an inhaler. Taking a pill at work or school feels different.
But here’s the problem: inhalers are expensive if you’re uninsured or underinsured. In the US, brand-name inhalers can cost $400 a month. In the UK, you pay a prescription fee unless exempt. That’s why 25% of asthma patients in the US ration their inhalers. That’s dangerous. Skipping doses leads to attacks. And attacks lead to ER visits.
Some people prefer pills because they’re easier. One tablet a day vs. remembering to use an inhaler twice daily, with proper technique. But the trade-off isn’t worth it. A Reddit user summed it up: “My inhaler takes 10 seconds. My prednisone made me gain 8 pounds and cry for no reason.”
What Should You Do?
If you have asthma, here’s your action plan:- Get diagnosed properly. Not all wheezing is asthma. Get a lung function test (spirometry).
- Find your triggers. Keep a diary for 4 weeks. Look for patterns.
- Use your inhaler correctly. Ask for a spacer. Get your technique checked by a nurse.
- Take your preventer inhaler every day-even if you feel fine.
- Know your rescue plan. If you’re using your reliever more than twice a week, see your doctor.
- If you’re on oral steroids regularly, ask: “Is there a better option?” Biologics might be available.
- Get your flu shot. Every year. No excuses.
Asthma isn’t a life sentence. With the right tools and knowledge, most people live full, active lives. The goal isn’t to be symptom-free every day-that’s unrealistic. The goal is to have control. To sleep through the night. To run up stairs without gasping. To not live in fear of the next attack.
That’s possible. But only if you understand your asthma-not just the symptoms, but the why behind them.
Can asthma go away on its own?
Some children outgrow asthma as their airways grow larger, especially if it’s mild and triggered mainly by colds. But in adults, asthma rarely disappears completely. Even if symptoms fade, the inflammation is still there. Stopping meds can bring it back. Always follow your doctor’s advice on when to adjust treatment.
Are inhalers addictive?
No. Inhalers don’t cause addiction. Reliever inhalers (like salbutamol) give quick relief because they open airways-they don’t change your brain chemistry. Preventer inhalers (steroids) reduce inflammation. Neither creates dependence. If you feel you need your inhaler too often, it means your asthma isn’t controlled-not that you’re addicted.
Can I use a nebulizer instead of an inhaler?
Nebulizers turn liquid medicine into a mist you breathe in. They’re useful for young children, people too weak to use inhalers, or during severe attacks. But for daily use, inhalers are faster, cheaper, and just as effective. Nebulizers take 10-15 minutes. Inhalers take 10 seconds. Most adults don’t need a nebulizer unless advised.
Why do I still wheeze even though I take my inhaler?
If you’re using your reliever inhaler regularly and still wheezing, your preventer inhaler might be too weak-or you’re not using it correctly. You might also have an undiagnosed trigger like allergies or GERD. See your doctor. You may need a higher dose, a combination inhaler, or a biologic.
Is it safe to use oral steroids for a long time?
No. Long-term oral steroids cause serious damage: bone loss, muscle weakness, diabetes, cataracts, and weight gain. They’re meant for short bursts-like 5-7 days during a flare-up. If you’re on them monthly or weekly, you need a different plan. Ask about biologics or higher-dose inhalers. There are safer options.
Can diet or supplements help with asthma?
No supplement or diet has been proven to replace asthma meds. But eating well supports overall lung health. Vitamin D deficiency is linked to worse asthma control-so get your levels checked. Omega-3s from fish may reduce inflammation slightly. Avoid processed foods and sugar, which can increase inflammation. But don’t rely on diet alone. Inhalers still work.
What’s the best way to track my asthma?
Use a peak flow meter daily. It measures how fast you can blow air out. Record your numbers. If your peak flow drops below 80% of your personal best, your asthma is worsening-even if you don’t feel symptoms yet. Smart inhalers (like Propeller or Hailie) can also track usage and alert you to triggers. Consistency matters more than perfection.
Next Steps: What to Do Today
If you have asthma:- Check your inhaler technique-ask your pharmacist or nurse to watch you use it.
- Review your reliever use. If it’s more than twice a week, book an appointment.
- If you’re on oral steroids, ask your doctor: “Is this the only option?”
- Get your flu shot if you haven’t already.
- Start a symptom diary. Note triggers, meds used, and sleep quality.
Asthma control isn’t about being perfect. It’s about being informed. You don’t need to avoid everything. You just need to know what matters-and how to protect yourself.


Doreen Pachificus
I’ve had asthma since I was 5, and honestly? The biggest game-changer was learning how to use my spacer. I used to just spray and hope. Now I actually feel the difference.
Also, never thought about how lying down at night makes mucus pool. That explains so much.
Thanks for this.