Cancer Treatment Comparison Tool
Treatment Selection
Select up to 3 treatments to compare their key characteristics for CLL treatment:
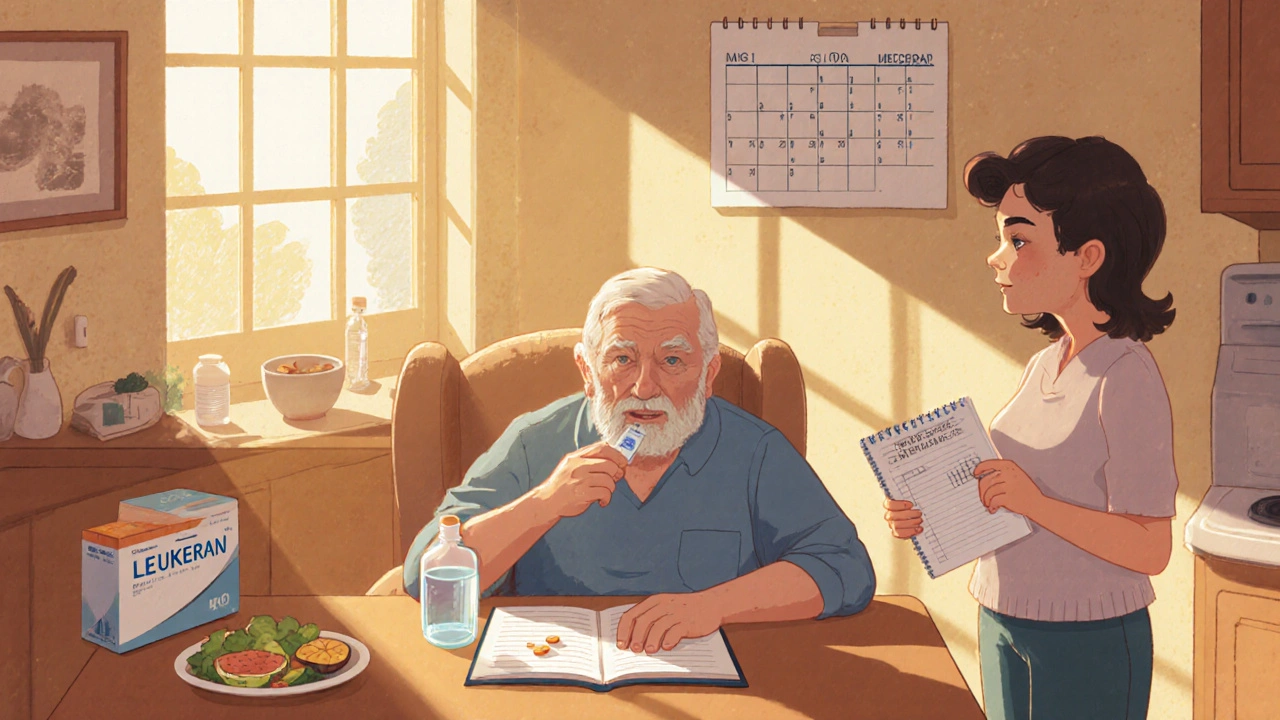
When you or a loved one faces a chronic‑lymphocytic leukemia (CLL) diagnosis, the first question is usually: which drug works best? Leukeran (chlorambucil) has been a go‑to oral chemotherapy for decades, but newer agents and older companions offer different benefits and trade‑offs. This guide walks through how Leukeran works, the most common alternatives, and a side‑by‑side comparison so you can talk to your oncologist with confidence.
What Leukeran (Chlorambucil) Actually Is
Leukeran (Chlorambucil) is an alkylating agent that interferes with DNA replication, ultimately causing cancer cells to die. It’s taken as a pill, making it convenient for patients who prefer oral therapy over IV infusions. Typical dosing starts at 0.1mg/kg daily for 14 days, followed by a rest period; the cycle repeats every 4-6 weeks. Because it’s older, the price is generally lower than newer biologics, and it’s covered by most insurance plans.
How Leukeran’s Mechanism Differs From Other Classes
Alkylating agents like Leukeran form cross‑links in DNA strands. This prevents the double helix from separating during replication, which stalls cell division. By contrast, many newer drugs target specific proteins or pathways (e.g., B‑cell receptor signaling) rather than causing broad DNA damage. That distinction matters for side‑effect profiles, response rates, and how long treatment can safely continue.
Common Alternatives to Leukeran
Below are the most frequently discussed options when doctors consider moving beyond or alongside Leukeran.
- Cyclophosphamide - another alkylating agent, usually given IV. It’s more potent but also carries higher risk of nausea and infection.
- Fludarabine - a purine analog that disrupts DNA synthesis. Often combined with cyclophosphamide and rituximab (the FCR regimen) for younger, fit patients.
- Rituximab - a monoclonal antibody that marks CD20‑positive B‑cells for destruction. It’s not a chemotherapy per se but works well in combination with others.
- Bendamustine - an alkylating agent with a distinct mechanism that also inhibits mitosis. Used in CLL and indolent non‑Hodgkin lymphoma.
- Vincristine - a vinca alkaloid that blocks microtubule formation. It’s rarely used alone for CLL but appears in combination protocols for other leukemias.
- Prednisone - a corticosteroid that reduces inflammation and can induce apoptosis in certain lymphoid cells. Often paired with other agents to improve response.
- Immunotherapy - newer checkpoint inhibitors (e.g., pembrolizumab) that unleash the immune system against cancer cells. Still experimental for CLL.
Side‑Effect Snapshot
Understanding toxicity helps you weigh benefits against everyday quality of life.
- Leukeran: mild nausea, fatigue, low‑grade myelosuppression, rare secondary cancers.
- Cyclophosphamide: more intense nausea, hemorrhagic cystitis (preventable with hydration), higher infection risk.
- Fludarabine: profound lymphopenia, opportunistic infections, possible neurotoxicity.
- Rituximab: infusion reactions, hepatitis B reactivation, modest neutropenia.
- Bendamustine: skin rash, alopecia, moderate neutropenia.
- Vincristine: peripheral neuropathy, constipation.
- Prednisone: weight gain, glucose intolerance, osteoporosis with long‑term use.
- Immunotherapy: immune‑related adverse events (colitis, dermatitis, pneumonitis).
Direct Comparison Table
| Drug | Class | Typical Indication in CLL | Administration | Key Side Effects | Typical Cost (US$) per 4‑week cycle |
|---|---|---|---|---|---|
| Leukeran (Chlorambucil) | Alkylating agent | First‑line for older or comorbid patients | Oral tablets | Low‑grade nausea, mild cytopenia | $150‑$250 |
| Cyclophosphamide | Alkylating agent | Often combined with other drugs for aggressive disease | IV infusion | Hemorrhagic cystitis, stronger myelosuppression | $500‑$800 |
| Fludarabine | Purine analog | Part of FCR regimen for fit patients | IV infusion | Severe lymphopenia, infection risk | $1,200‑$1,800 |
| Rituximab | Monoclonal antibody | Combined with chemo or as single‑agent for CD20+ disease | IV infusion | Infusion reactions, hepatitis B reactivation | $2,000‑$3,000 |
| Bendamustine | Alkylating agent | Alternative to FCR for older patients | IV infusion | Rash, moderate neutropenia | $1,500‑$2,200 |
How to Decide Which Option Fits Your Situation
Choosing a drug isn’t just about numbers; it’s a personal balance of health status, lifestyle, and goals.
- Age and comorbidities. Older patients or those with heart, kidney, or liver issues often stay on Leukeran because it’s gentler and oral.
- Desired speed of response. If you need a rapid reduction in lymphocyte count, combinations like FCR (fludarabine+cyclophosphamide+rituximab) act faster than Leukeran alone.
- Travel and infusion logistics. Oral therapy means fewer trips to the infusion center, which can be a big quality‑of‑life factor.
- Financial considerations. Out‑of‑pocket costs still matter. Even with insurance, a high‑deductible plan might make Leukeran the most affordable choice.
- Potential for long‑term toxicity. Alkylators carry a small risk of secondary malignancies years later. Targeted agents can cause unique immune‑related issues.
Talk with your hematologist about these factors. Bring a list of your current meds, any past infections, and a realistic schedule of clinic visits.
Practical Tips for Managing Side Effects
- Stay hydrated. Hydration reduces the chance of bladder irritation from alkylators.
- Use anti‑nausea meds. Over‑the‑counter dimenhydrinate works for most mild cases; prescription ondansetron is an option for stronger symptoms.
- Monitor blood counts. Labs every 2‑4 weeks let your doctor catch neutropenia early and adjust dose.
- Vaccinate wisely. Avoid live vaccines while on immunosuppressive chemo; inactivated flu vaccine is safe.
- Get a support buddy. Having someone to track appointments and side‑effect logs saves stress.
Key Takeaways
- Leukeran is an oral alkylating agent that’s cost‑effective and well‑tolerated for many older CLL patients.
- Alternatives like cyclophosphamide, fludarabine, rituximab, and bendamustine offer higher potency but bring more intense side effects and infusion requirements.
- Match the drug to your age, comorbidities, lifestyle, and financial situation - no single answer fits everyone.
- Regular labs, hydration, and anti‑nausea measures keep side effects manageable regardless of the chosen therapy.
Frequently Asked Questions
Is Leukeran still used as a first‑line therapy in 2025?
Yes. Guidelines from the NCCN and ESMO still list oral chlorambucil (Leukeran) as a first‑line option for older or less‑fit CLL patients, especially when combined with a CD20 antibody like obinutuzumab.
How does the efficacy of Leukeran compare to the FCR regimen?
FCR (fludarabine+cyclophosphamide+rituximab) typically yields higher complete remission rates (30‑40%) and longer progression‑free survival than Leukeran alone (10‑15%). However, FCR also carries more severe myelosuppression and is usually reserved for patients under 70 with good organ function.
Can I switch from Leukeran to another drug if the disease progresses?
Absolutely. Many oncologists start with Leukeran, then move to a more aggressive regimen like bendamustine+rituximab or newer BTK inhibitors if the cancer becomes resistant. The transition is decided based on lab results and symptom changes.
What are the most common drug‑drug interactions with Leukeran?
Because Leukeran is metabolized by the liver’s CYP2C9 pathway, caution is needed with strong inhibitors like fluconazole or NSAIDs that can increase toxicity. Always list every prescription and supplement to your pharmacist.
Is there any dietary advice while taking Leukeran?
No strict diet is required, but a balanced diet rich in fruits, vegetables, and protein helps maintain blood counts. Avoid grapefruit juice, which can interfere with liver enzymes.


Maureen Crandall
Leukeran’s cheap price makes it a solid fallback for budget‑tight patients.