Medication Interaction Checker
Check for Potential Interactions
This tool shows common interactions between medications and foods/supplements. It is not a substitute for professional medical advice.
Every year, over a million people in the U.S. are injured because of medication errors-and a big chunk of those are due to drug interactions you never saw coming. You might think your pharmacist just hands out pills, but they’re actually trained to spot hidden dangers between your prescriptions, supplements, even your morning grapefruit juice. The problem? Most people never ask. And that’s where things go wrong.
Why Medication Interactions Are More Common Than You Think
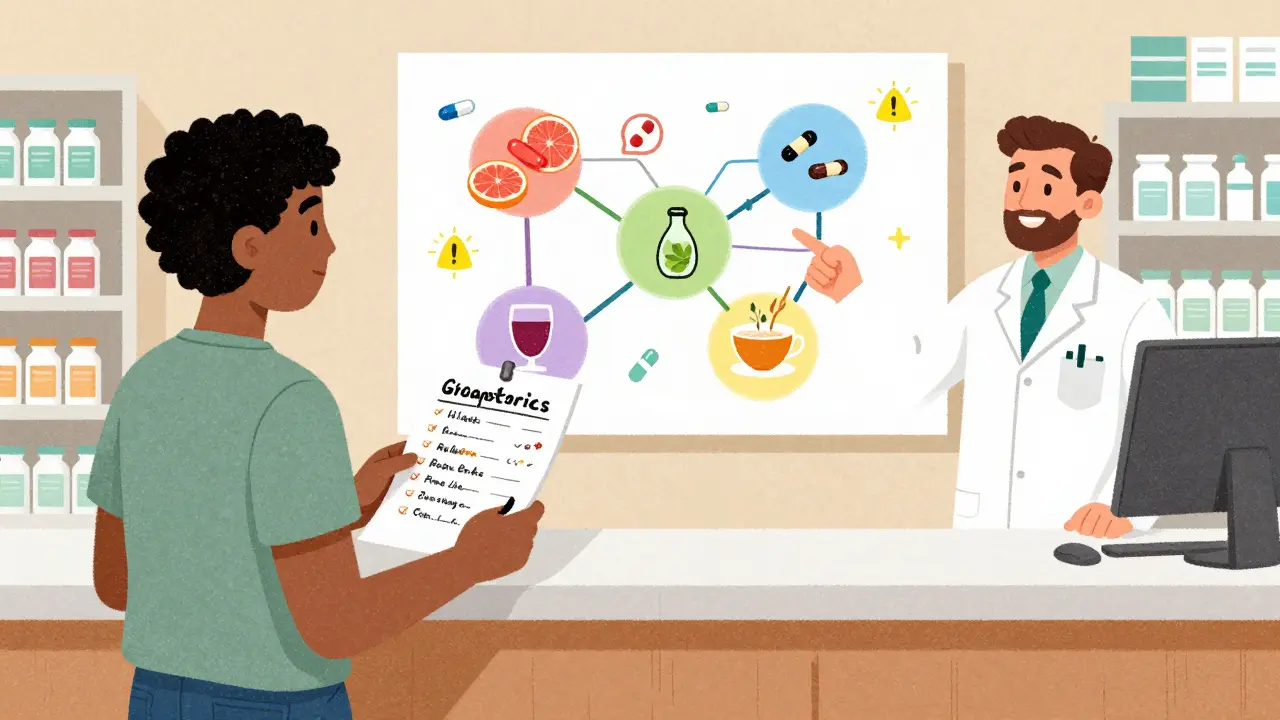
You take your blood pressure pill. You grab a cold medicine off the shelf. You start taking turmeric for inflammation. You drink your usual glass of grapefruit juice with breakfast. None of that seems dangerous on its own. But together? That’s where the risk spikes. Pharmacists see this every day. A 2023 report from the American Society of Health-System Pharmacists found that only 38% of patients get proper counseling about interactions when picking up a new prescription. That means over 60% are walking out with no idea they might be mixing something dangerous. Some interactions are silent. Warfarin, a blood thinner, can become too strong if you start taking cranberry juice or vitamin K supplements. One study showed 37% of people on warfarin didn’t know this. Another common trap: levothyroxine, used for thyroid issues, loses up to half its effectiveness if taken with calcium supplements-unless you space them out by four hours. Then there’s grapefruit juice. It doesn’t just affect one or two drugs. It messes with around 85 prescription medications, including statins like atorvastatin. One study found that drinking grapefruit juice with these pills can spike blood levels by up to 1,500%. That’s not a minor side effect-that’s a hospital visit waiting to happen.What Kind of Interactions Should You Be Worried About?
Not all interactions are the same. Here’s what to watch for:- Drug-drug: Two prescriptions clashing. Like mixing an SSRI (like fluoxetine) with an MAOI (an older antidepressant). This combo can trigger serotonin syndrome-a rare but life-threatening condition that causes high fever, rapid heartbeat, and confusion.
- Drug-supplement: Herbal products aren’t harmless. St. John’s wort can make birth control, antidepressants, and even some heart meds stop working. A 2022 study showed herbal supplement use jumped nearly 24% in just one year.
- Drug-food: Grapefruit juice is the big one, but antacids like Tums can block absorption of certain Hepatitis C drugs. Dairy products can interfere with antibiotics like tetracycline.
- Drug-beverage: Alcohol is a silent player. It can make medications like metronidazole cause nausea, vomiting, and a pounding heart. Even if you don’t drink often, a single glass can be risky with certain drugs.
- Drug-environment: Some meds make you more sensitive to sunlight. Antibiotics, diuretics, even some acne treatments can cause severe sunburn or skin discoloration. You won’t know unless you ask.
What to Ask Your Pharmacist-The Exact Questions That Matter
Don’t wait for them to bring it up. Pharmacists are busy. You need to lead the conversation. Here are the exact questions to ask when you pick up any new medication:- "Does this medication interact with anything else I’m taking?" This includes every prescription, over-the-counter pill, vitamin, herb, or supplement. Don’t leave anything out-even if it seems "natural."
- "Are there foods, drinks, or beverages I should avoid?" Grapefruit juice is the classic, but don’t forget alcohol, dairy, caffeine, or even high-fiber meals that can slow absorption.
- "Can this affect my other health conditions?" For example, a decongestant might raise your blood pressure. A painkiller might stress your kidneys if you have diabetes.
- "What are the warning signs if something’s going wrong?" What symptoms should make you call your doctor or go to the ER? Dizziness? Rapid heartbeat? Unusual bruising? Know the red flags.
- "Do I need to space this out from other meds?" Timing matters. Levothyroxine should be taken on an empty stomach, at least 4 hours before or after calcium, iron, or antacids.
- "Will I need any blood tests or monitoring while taking this?" Some drugs need regular checks-like warfarin requiring INR tests. If you’re on a statin, liver enzymes might need tracking.
- "Is there a cheaper or generic version that won’t change how this interacts?" Sometimes switching brands can alter how a drug is absorbed. Your pharmacist can tell you if a generic is truly equivalent.

How to Prepare Before You Walk In
You won’t remember everything if you’re winging it. Bring this to your pharmacy visit:- A written list of every medication you take-prescriptions, OTCs, vitamins, supplements, herbal teas, even CBD oil.
- The dosage and timing for each (e.g., "20 mg of lisinopril every morning," "500 mg of vitamin C at lunch").
- Any recent changes-new prescriptions, skipped doses, or symptoms you’ve noticed.
- Your biggest concern: "I’ve been feeling dizzy since I started this new pill. Could it be the interaction?"
What If Your Pharmacist Doesn’t Offer Info?
It’s not your fault if they don’t bring it up. Pharmacists are stretched thin. But you have a right to know. If they seem rushed or dismissive, say: "I’ve heard that some medications can interact in ways that aren’t obvious. Could we take a minute to check mine?" Most will pause and help. If they still don’t, ask for a consultation. Many pharmacies offer free 10-15 minute sessions just for this. Or ask if they can email you a summary of interactions after your visit. And if you’re still unsure? Call back. Or visit another pharmacy. Your safety isn’t something to gamble on.
What Happens After You Get the Info?
Knowledge is only useful if you act on it.- Set phone alarms for medication timing if spacing is needed.
- Keep a small note in your wallet or phone: "Avoid grapefruit with my statin."
- Report any side effects-even if you’re not sure it’s the drug. The FDA’s MedWatch program lets you report directly through their app. Over 12,000 reports came in through the app in just six months in 2023.
- Share your interaction list with your doctor every visit. Pharmacists and doctors need to be on the same page.
Why This Matters More Than Ever
More people are taking multiple medications than ever before. The average American adult takes four prescription drugs. Add supplements, OTCs, and lifestyle habits-and the chance of a hidden interaction skyrockets. Pharmacists have the training. They’ve spent years learning how drugs behave in the body. But they can’t help if you don’t tell them what you’re taking-or if you don’t ask the right questions. The system is set up to catch major errors. Automated systems screen for dangerous combos. But they can’t know about your herbal tea, your weekend wine, or the magnesium you started last week. That’s where you come in.Final Thought: You’re the Key
You’re the only one who knows your whole routine. Your pharmacist can’t read your mind. But they can protect you-if you give them the full picture. Next time you pick up a prescription, don’t just say "thanks." Ask the questions. Write them down. Bring your list. Make sure you walk out knowing exactly what to avoid-and what to watch for. Because in the end, safety isn’t about luck. It’s about asking the right questions at the right time.Can I just check medication interactions online instead of asking my pharmacist?
Online tools can help, but they’re not enough. Apps and websites might miss interactions with supplements, herbal products, or specific timing issues. A 2023 study found pharmacy apps only caught 63% of serious interactions. Pharmacists have access to your full medical history, know your exact dosages, and can spot risks that automated systems miss. Use apps as a backup-not a replacement.
What if I’m taking a lot of medications? Should I still ask?
Yes-and even more so. The more medications you take, the higher the chance of a hidden interaction. People on five or more drugs are at the highest risk. Pharmacists are trained to handle complex regimens. Ask for a comprehensive medication review. Medicare Part D even covers this annually for qualifying patients. Don’t assume it’s too complicated-they’ve seen it all before.
Do over-the-counter meds really interact with prescriptions?
Absolutely. Many people think "OTC" means "safe," but that’s not true. Painkillers like ibuprofen can increase bleeding risk if you’re on blood thinners. Decongestants in cold meds can raise blood pressure. Antacids can block absorption of thyroid meds and antibiotics. Always include every OTC product on your list-even the ones you only take once in a while.
Can supplements like fish oil or vitamin D interact with my meds?
Yes. Fish oil can thin the blood, which can be dangerous if you’re on warfarin or aspirin. Vitamin D can raise calcium levels, which may interfere with heart medications. Even something as simple as vitamin K can undo the effects of blood thinners. Never assume a supplement is harmless. Always list it when you talk to your pharmacist.
What if I forget to take my medication and then take it later? Could that cause an interaction?
It can. Taking two doses too close together can overload your system, especially with drugs that have narrow safety margins-like blood thinners or seizure meds. Some meds need to be taken at specific times to avoid interactions with food or other drugs. If you miss a dose, ask your pharmacist what to do. Don’t just double up unless they say it’s safe.
Can my pharmacist help me switch to a safer medication if interactions are a problem?
Yes. Pharmacists can suggest alternative drugs that work similarly but have fewer interactions. For example, if grapefruit juice is a problem with your statin, they might recommend rosuvastatin instead, which isn’t affected by grapefruit. They can also check for lower-cost generics that are equally safe. Always ask-they’re there to help you find the best option.
Is it safe to take my meds with alcohol if I only drink occasionally?
Not always. Even one drink can trigger a reaction with certain drugs. Metronidazole, some antidepressants, and sleep aids can cause nausea, dizziness, or heart issues with just a small amount of alcohol. The National Institute on Alcohol Abuse and Alcoholism says over 40% of adults take medications that interact with alcohol. If you’re unsure, assume it’s unsafe until your pharmacist says otherwise.
Should I bring my pill bottles to the pharmacy?
Yes. Bottle labels show exact names, dosages, and instructions. Sometimes people misremember what they’re taking. Seeing the bottle helps the pharmacist confirm everything is correct. If you can’t bring them, at least take clear photos of the labels with your phone.
Can pharmacists tell me if my meds are safe during pregnancy or breastfeeding?
Yes. Pharmacists are trained to assess medication safety during pregnancy and breastfeeding. They can tell you which drugs are known to be safe, which to avoid, and which have limited data. If you’re pregnant or nursing, always mention it when picking up any new medication-even if your doctor didn’t bring it up.
What if I get a new prescription from a different doctor? Should I still check with my pharmacist?
Always. Each doctor might only see part of your picture. Your pharmacist sees your full list. A new painkiller from your orthopedist might interact with your heart medication prescribed by your cardiologist. Never assume your doctors have shared everything. Your pharmacist is your safety net.

Phil Hillson
bro i took ibuprofen with my blood thinner once and thought i was gonna die lol my heart was racing like a damn racecar and i had to call 911 pharmacist was like 'uh yeah that's a thing' thanks for nothing