Diabetes Alcohol Safety Calculator
Drinking alcohol while taking diabetes meds isn’t just a bad idea-it can be dangerous. For many people with diabetes, a glass of wine or a beer seems harmless. But when alcohol meets medications like insulin or metformin, your body doesn’t know what to prioritize: lowering blood sugar or detoxifying alcohol. And that confusion can land you in the hospital.
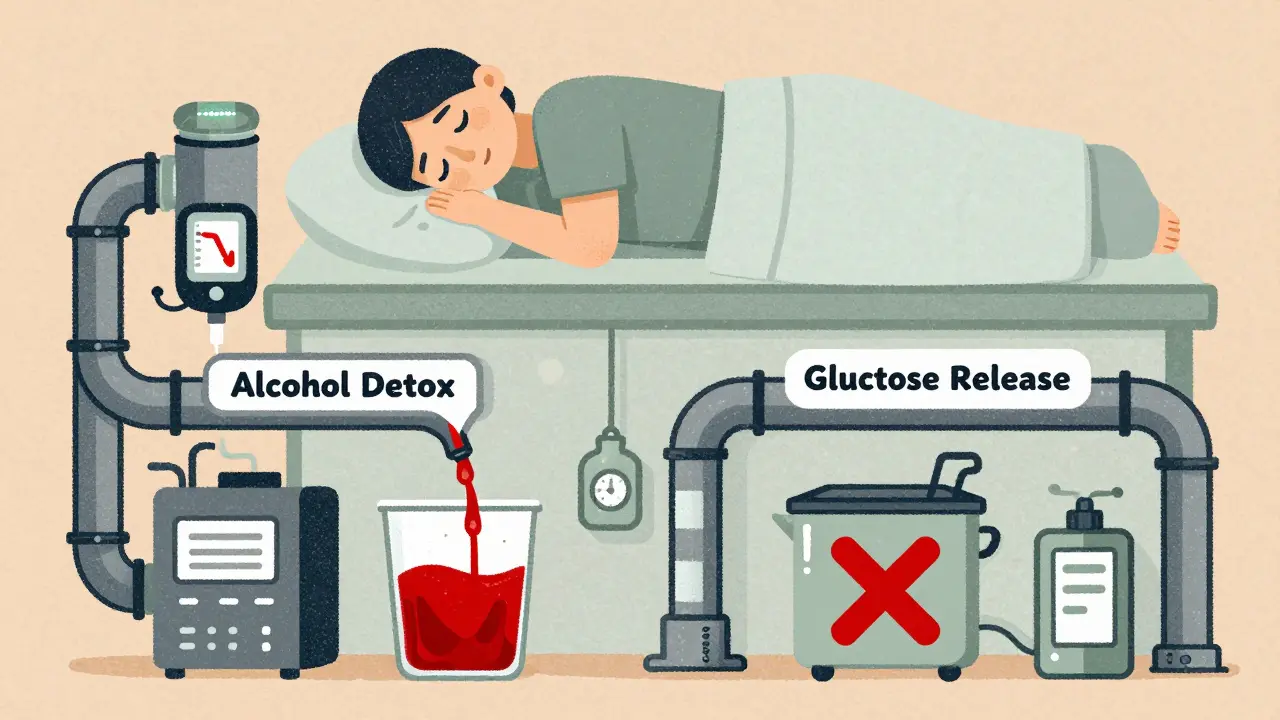
Why Alcohol Triggers Dangerous Low Blood Sugar
Your liver is busy 24/7. It stores glucose when you’ve eaten too much and releases it when you haven’t eaten in a while. But when alcohol enters the picture, the liver drops everything else to deal with it. That’s because alcohol is toxic, and your body treats it like an emergency. So instead of releasing glucose to keep your blood sugar stable, the liver shuts down that function to focus on breaking down alcohol. This is why your blood sugar can crash hours after your last drink-especially if you drank on an empty stomach. People on insulin or sulfonylureas are at highest risk. These meds already push your blood sugar down. Alcohol doesn’t just add to that-it blocks your body’s natural safety net. Here’s the scary part: the signs of low blood sugar-dizziness, confusion, slurred speech, sweating, weakness-look exactly like being drunk. If you pass out after a few drinks, a bystander might assume you’re just intoxicated. They won’t know you need glucose, not more vodka. That delay can be deadly. A 2023 study from the American Diabetes Association found that nearly 40% of people with type 1 diabetes who drank alcohol experienced nighttime hypoglycemia, even if their blood sugar was fine before bed. Some didn’t wake up. Others needed emergency glucagon injections.Metformin and Alcohol: A Silent Threat to Your Liver
Metformin is the most common diabetes pill worldwide. It’s safe for most people-but not when mixed with alcohol. Both metformin and alcohol are processed by the liver. Together, they overload it. Over time, this can lead to fatty liver disease, inflammation, or even a rare but life-threatening condition called lactic acidosis. Lactic acidosis happens when your body makes too much lactic acid and can’t clear it. Metformin already slightly increases lactic acid production. Alcohol slows down how fast your liver removes it. The result? Acid builds up in your blood. Symptoms include nausea, vomiting, muscle pain, rapid breathing, and extreme fatigue. If ignored, it can lead to organ failure. Even moderate drinking-two drinks a night-can raise this risk if you have other health problems like kidney disease or liver damage. And here’s the twist: many people don’t know they have early liver damage. By the time symptoms show up, it’s often too late. The FDA recalled some extended-release metformin tablets in 2020 due to a cancer-causing contaminant. While that’s unrelated to alcohol, it reminds us: medication quality matters. If your metformin isn’t from a trusted source, adding alcohol makes the risk even higher.What Drinks Are Safer? And What to Avoid
Not all alcohol is created equal. Sugary cocktails, sweet wines, and regular beer spike your blood sugar first-then crash it later when the liver finally gets around to metabolizing the alcohol. That rollercoaster is worse than just drinking straight liquor. Here’s what works better:- Light beer (under 10g carbs per bottle)
- Dry white or red wine (no added sugar)
- Hard seltzers with no added sugar
- Distilled spirits (vodka, gin, whiskey) mixed with soda water and lime
- Margaritas, piña coladas, and other sugary cocktails
- Regular soda, juice, or tonic water as mixers
- Sweet dessert wines and liqueurs
- Beer with high carbs (some craft beers have 20+g carbs per serving)

How to Drink Safely-If You Choose To
The American Diabetes Association says there’s no one-size-fits-all rule. But if you’re going to drink, follow these steps:- Never drink on an empty stomach. Eat a meal with carbs and protein first. A sandwich, rice, or even a banana helps.
- Check your blood sugar before you start. If it’s below 100 mg/dL, don’t drink. Wait until it’s stable.
- Limit yourself. One drink for women, two for men per day. That’s it. More than that? The risks rise fast.
- Check your blood sugar every 1-2 hours while drinking. And again before bed. Alcohol can cause lows for up to 12 hours later.
- Wear a medical ID. It tells emergency responders you have diabetes. That could save your life.
- Tell someone you’re with. Make sure a friend knows your symptoms of low blood sugar. They might be the only one who notices you’re in trouble.
Who Should Avoid Alcohol Completely?
Some people shouldn’t drink at all:- Those with a history of severe hypoglycemia or unawareness (you don’t feel the warning signs)
- People with liver disease, including fatty liver or cirrhosis
- Anyone taking insulin or sulfonylureas who struggles to manage blood sugar
- Those with kidney disease or pancreatitis
- People who’ve had lactic acidosis before

What Your Doctor Should Tell You
A 2021 study in the Journal of Diabetes Science and Technology found that only 43% of primary care doctors routinely ask diabetic patients about alcohol use. That’s a huge gap. You shouldn’t have to bring it up first. Your doctor should discuss:- Which of your meds are risky with alcohol
- Your personal risk for hypoglycemia
- Your liver and kidney health
- Whether your CGM can help track alcohol-related lows
The Bigger Picture: Alcohol and Long-Term Diabetes Health
Heavy drinking-five or more drinks a day for men, four for women-is linked to worse diabetes control. It increases insulin resistance, raises triglycerides, and damages the pancreas. Over time, that means more nerve damage, more heart disease, and more kidney problems. But here’s the twist: some studies show that *moderate* drinking (one drink a day) might lower heart disease risk in people with type 2 diabetes. That’s why blanket “no alcohol” rules don’t always make sense. It’s about balance. The key is personalization. Your age, weight, meds, liver health, and drinking habits all matter. There’s no universal answer. But there is a universal warning: alcohol doesn’t play nice with diabetes meds.What’s New in 2026
New continuous glucose monitors (CGMs) like the Dexcom G7 and FreeStyle Libre 3 now detect patterns linked to alcohol use-even if they can’t measure alcohol directly. If your sugar drops sharply after 10 p.m. and you drank earlier, the app might flag it as “possible alcohol effect.” The Joslin Diabetes Center is running a 12-month study tracking how moderate drinking affects liver function in people on metformin. Results are due late 2024. Early data suggests even one drink a day can slow liver recovery in people with early fatty liver. Meanwhile, diabetes educators are now trained to talk about alcohol like they do about sugar or carbs. In 2022, 89% of certified diabetes educators included alcohol in patient education. That’s progress. But you still have to be your own advocate. No app or doctor can replace knowing your body’s signals.Can I drink alcohol if I take metformin?
You can, but only with extreme caution. Metformin and alcohol both stress the liver. Together, they raise your risk of lactic acidosis-a rare but dangerous condition. Stick to one drink max, always eat food first, and avoid drinking if you have liver or kidney problems. If you’re unsure, get your liver enzymes checked.
Why does alcohol cause low blood sugar hours after drinking?
Your liver stops releasing glucose to focus on breaking down alcohol. This can last for hours, even after you’ve stopped drinking. If you’re on insulin or sulfonylureas, your body has no backup system to raise blood sugar. That’s why lows happen at night-sometimes while you’re asleep.
Is red wine safer than beer for people with diabetes?
Yes, dry red wine is generally safer than beer. Beer has more carbs and can spike blood sugar before causing a crash. Dry wine has less sugar and fewer carbs. But it still affects your liver. Stick to one 5-ounce glass and eat food with it.
Can I use my CGM to detect alcohol-related low blood sugar?
Your CGM won’t detect alcohol directly, but it can show you patterns. If your glucose drops sharply after drinking-even if you didn’t eat-it’s likely alcohol-related. Many CGM apps now flag “possible alcohol effect” based on timing and trends. Use that data to adjust your habits.
What should I do if I feel dizzy after drinking and think I’m low?
Check your blood sugar immediately. Don’t assume you’re just drunk. If your sugar is below 70 mg/dL, take 15g of fast-acting carbs-glucose tablets, juice, or candy. Wait 15 minutes and check again. If you can’t check, assume you’re low and treat anyway. Tell someone nearby you have diabetes. If symptoms worsen or you can’t wake up, call emergency services.
If you’re thinking about cutting back or quitting alcohol entirely, you’re not alone. Many people with diabetes find that once they stop, their blood sugar becomes easier to manage, their energy improves, and their liver enzymes return to normal. It’s not about perfection-it’s about protecting your future.

Faith Wright
So let me get this straight-you’re telling me I can’t have my Friday wine because my liver’s too busy playing detox janitor? Thanks, I guess I’ll just start drinking water and calling it a ‘wellness ritual’.