Medication Side Effect Assessment Tool
Step 1: Select your symptom
Choose the side effect you're experiencing to get specific guidance.
Step 2: Check if your medication requires tapering
Some medications are dangerous to stop suddenly. Have you been taking any of these?
Important: Do not stop suddenly
Medications like beta blockers, benzodiazepines, clonidine, and antidepressants can cause severe withdrawal symptoms if stopped abruptly. Contact your healthcare provider immediately to develop a tapering plan.
It’s one thing to feel a little dizzy or nauseous when you start a new medication. It’s another when your body starts shutting down. Not every side effect means you should quit the drug. But some do - and waiting even a few hours could cost you your life.
Millions of people take prescription drugs every day. Most handle the side effects fine. A dry mouth, a headache, a bit of fatigue - these often fade after a week or two. But when a reaction turns severe, the clock starts ticking. The difference between a manageable annoyance and a medical emergency isn’t just about how bad it feels. It’s about what’s happening inside your body.
Life-Threatening Reactions: Stop Now, Ask Questions Later
There are side effects that demand immediate action. No waiting. No calling your doctor tomorrow. If you experience any of these, stop the medication right away and get emergency help:
- Anaphylaxis: Swelling of the throat, trouble breathing, rapid heartbeat, hives, or a sudden drop in blood pressure. This can happen within minutes. Penicillin is the most common trigger, but many antibiotics, NSAIDs, and even some vaccines can cause it. About 1 in 10,000 people experience drug-induced anaphylaxis - and it kills 1 in 5 if not treated fast.
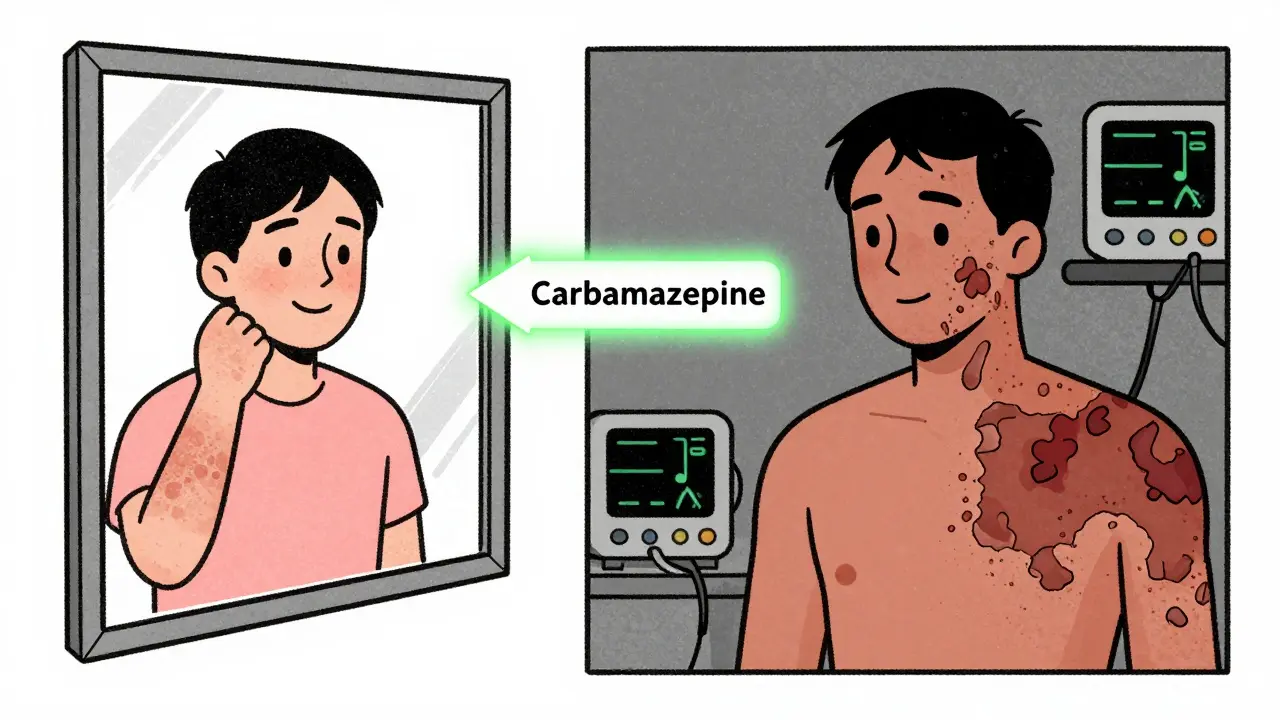
- Stevens-Johnson Syndrome (SJS) or Toxic Epidermal Necrolysis (TEN): A rash that turns into blisters, peeling skin, and sores in the mouth, eyes, or genitals. SJS has a 5-15% death rate. TEN? Up to 50%. Drugs like carbamazepine, lamotrigine, allopurinol, and sulfa antibiotics are the usual suspects. If you notice a spreading rash with blistering, especially within the first few weeks of starting a new drug, get to an ER immediately.
- Acute liver failure: Yellowing of the skin or eyes, dark urine, extreme fatigue, or belly pain. Medications like isoniazid (used for TB), acetaminophen (in high doses), and some antibiotics can damage the liver. If liver enzymes (ALT) rise more than 3 times the normal level and you have symptoms - stop the drug. No exceptions.
- Agranulocytosis: A sudden drop in white blood cells. You’ll feel like you’ve got the flu - fever, sore throat, chills. It’s rare, about 1 in a million, but if you don’t stop the drug fast, your body can’t fight infection. Mortality hits 5-10% if untreated.
These aren’t "wait and see" situations. They’re emergency signals. The FDA classifies them as serious adverse events - meaning they can lead to death, hospitalization, or permanent disability. That’s why black box warnings exist. For example, carbamazepine carries a warning for people with the HLA-B*1502 gene variant (common in Asian populations). If you have that gene and get a rash, stopping the drug immediately cuts your risk of SJS by over 90%.
Not All Side Effects Are Created Equal
Just because a side effect is unpleasant doesn’t mean you should quit. Many patients stop their meds because they feel off - only to replace one problem with another.
Take statins. About 10% of people report muscle pain. But studies show only 5% of those cases are true statin-induced myopathy. The rest? Could be from aging, lack of movement, or another drug. Stopping without checking could mean missing out on a medication that cuts your heart attack risk by 30%. Always talk to your doctor before quitting.
Same goes for antidepressants. If you’re on an SSRI and feel nauseous, jittery, or have weird dreams - those are common in the first few weeks. But if you stop cold turkey, 20-50% of people develop withdrawal symptoms: brain zaps, dizziness, anxiety, even seizures. A 2023 FDA update now requires manufacturers to include specific tapering schedules on SSRI labels. Why? Because structured weaning reduces withdrawal severity by 73%.
The Hidden Danger: Stopping the Wrong Way
Some medications are dangerous to quit suddenly - even if you’re suffering. Stopping them can trigger worse problems than the original side effect.
- Beta blockers: If you’re on propranolol or metoprolol for high blood pressure or heart disease, stopping abruptly can spike your heart rate and blood pressure. In patients with coronary artery disease, this raises heart attack risk by 300% in the first week.
- Benzodiazepines: Drugs like Xanax or Valium. Stopping suddenly can cause seizures, hallucinations, or extreme anxiety. Long-term users have a 10-15% chance of withdrawal seizures if they quit cold turkey.
- Clonidine (Catapres): Used for high blood pressure. Quitting fast can cause rebound hypertension - your blood pressure surges to dangerous levels. One study found 30-40% of patients had hypertensive emergencies after stopping clonidine without tapering.
- Antidepressants (especially SSRIs and SNRIs): Withdrawal isn’t just "feeling off." It can include electric shock sensations, nausea, insomnia, and suicidal thoughts. The risk is highest with short-half-life drugs like paroxetine or venlafaxine.
These aren’t rare. The American Medical Association says 1.3 million ER visits a year in the U.S. are from adverse drug events - and about a third of those are from improper discontinuation. That’s not just bad luck. It’s a failure to understand the balance between side effects and withdrawal risks.
How to Decide: The 5-Question Framework
Doctors and pharmacists use a simple, proven system to decide whether to stop a drug or taper it. Here’s how it works:
- Is it life-threatening? If yes - stop immediately. Anaphylaxis, SJS, liver failure, agranulocytosis - no hesitation.
- Is this a drug that causes withdrawal if stopped suddenly? If yes - don’t quit cold turkey. Call your provider. You’ll need a taper plan.
- Are there safer alternatives? Maybe switching to a different drug in the same class avoids the side effect. For example, if you’re allergic to penicillin, amoxicillin might still be safe. Or if statins cause muscle pain, switching to rosuvastatin often helps.
- What’s the risk of continuing vs. stopping? Is the drug keeping you alive? Preventing stroke? Controlling seizures? Sometimes the side effect is worse than the disease.
- Do you understand the risks? Many patients stop meds because they’re scared. But fear isn’t a medical reason. A clear conversation with your provider is.
This framework was tested in over 1,200 patients. It worked 92% of the time. Standard care? Only 67%. The difference? Structure. Clarity. Knowledge.

What to Do Right Now
If you’re worried about a side effect:
- Don’t stop the drug unless it’s one of the life-threatening reactions listed above.
- Take a photo of any rash, swelling, or unusual symptoms. This helps your doctor diagnose faster.
- Call your prescriber or pharmacist. Don’t wait. Don’t Google. Don’t rely on Reddit threads.
- Keep a log: When did the side effect start? What did you take? How bad is it on a scale of 1-10? This helps spot patterns.
- If you’re on blood pressure meds, beta blockers, antidepressants, or benzodiazepines - never stop without a plan.
Here’s the hard truth: 42% of patients stop their meds without talking to anyone. And 18% of them end up in the hospital because of it. You don’t have to be one of them.
Bottom Line
Side effects aren’t always a reason to quit. But some are. The key isn’t just knowing what’s dangerous - it’s knowing what’s dangerous to stop. Anaphylaxis? Stop now. Muscle pain on statins? Talk to your doctor. Dizziness on blood pressure meds? Maybe adjust the dose. Panic when quitting antidepressants? Taper slowly.
Medications save lives. But they can also hurt you - if you don’t handle them right. The goal isn’t to avoid side effects at all costs. It’s to avoid the bigger dangers: untreated disease, withdrawal crises, and preventable deaths.
When in doubt - don’t guess. Call your provider. Your body is giving you signals. Learn how to read them.
What side effects mean I should stop my medication right away?
Stop immediately if you experience anaphylaxis (trouble breathing, swelling, hives), Stevens-Johnson Syndrome or toxic epidermal necrolysis (blistering rash, peeling skin), signs of acute liver failure (yellow skin, dark urine, severe pain), or agranulocytosis (fever, sore throat, chills). These are life-threatening and require emergency care.
Can I stop my antidepressant if I feel worse?
No. Feeling nauseous, anxious, or having "brain zaps" in the first few weeks is common and usually passes. Stopping suddenly can trigger severe withdrawal symptoms - including seizures or suicidal thoughts. Talk to your doctor. A slow taper reduces withdrawal risk by over 70%.
Why is it dangerous to stop blood pressure meds suddenly?
Stopping beta blockers or clonidine abruptly can cause rebound hypertension - your blood pressure spikes dangerously high. This can trigger heart attack, stroke, or organ damage. Studies show 30-40% of patients who quit these drugs without tapering end up in the ER. Always follow a doctor-approved taper plan.
What if I have a rash but I’m not sure if it’s serious?
If the rash is spreading, blistering, or involves your mouth, eyes, or genitals - go to the ER. If it’s mild and localized, call your doctor. Don’t wait. Drugs like carbamazepine and lamotrigine can cause fatal skin reactions within days. Early recognition saves lives.
How common are serious side effects from medications?
Serious side effects are rare but deadly. Anaphylaxis happens in 1-15 per 10,000 users. SJS/TEN occurs in 1-2 per million. Liver failure from drugs like isoniazid affects about 1 in 10,000. But because so many people take medications, these events add up - causing over 1.3 million ER visits in the U.S. each year.

