When you’re scheduled for surgery, the last thing you want is a preventable reaction to a drug you’ve taken before. Yet every year, thousands of patients experience serious complications because their past drug reactions weren’t clearly communicated. It’s not always about being allergic - sometimes it’s about side effects, intolerances, or past bad experiences that were never properly documented. But here’s the truth: drug reactions before surgery are one of the most preventable causes of surgical emergencies. If you’ve ever had a bad reaction to medicine, you need to know exactly how to talk about it - and when to speak up.
Why This Matters More Than You Think
A 2022 NIH study found that 4.5% of all surgical complications are linked to medication errors. Of those, about 1.1% of anesthesia-related deaths are tied to allergic reactions. That might sound rare, but when you’re the patient, it’s not a statistic - it’s your life. The good news? Hospitals that use clear, standardized communication protocols cut these errors by 37%. That’s not magic. That’s just good process. The problem isn’t usually the doctors. It’s the gap between what you remember and what gets written down. Patients often say, “I’m allergic to penicillin,” when they actually had a rash or nausea. Or they forget about that one time they got sick after a dental procedure and took codeine. Or they don’t realize that supplements like St. John’s Wort or fish oil can interact with anesthesia. These aren’t small details. They’re critical.What Counts as a Drug Reaction?
Not every bad feeling after a drug is an allergy. Here’s how to tell the difference:- Allergy: Immune system response - hives, swelling, trouble breathing, drop in blood pressure, anaphylaxis. These can be life-threatening.
- Intolerance or side effect: Nausea, dizziness, headache, itching without rash. Not immune-related, but still dangerous if repeated.
- Drug interaction: Reaction caused by mixing meds - like taking an MAOI antidepressant and then getting ephedrine during surgery, which can spike your blood pressure dangerously.
Start Early - Don’t Wait Until the Day Before
The ideal time to start talking about your drug history is at least 72 hours before surgery. That’s not a suggestion - it’s standard protocol at top hospitals like Mayo Clinic and Stanford. Why? Because your surgeon and anesthesiologist need time to review your history, consult with pharmacists, and adjust your plan. Most people wait until the pre-op nurse asks them in the holding area. That’s too late. You’re nervous. You’re rushed. You might not remember what you took five years ago. By then, it’s too late to call in an allergist or switch to a safer drug. Here’s what you should do:- Get your medication list together - prescriptions, over-the-counter drugs, vitamins, herbal supplements, and even CBD or melatonin.
- Write down every reaction you’ve ever had. Include the drug name, when it happened, what symptoms you felt, how long they lasted, and what treatment you got.
- Bring any old medical records or allergy cards you have.
- Call your primary care doctor or pharmacist and ask them to help you review your list. They’ve seen your full history.
Use the Right Words - Don’t Say “Allergic” Unless You Mean It
A nurse on AllNurses.com shared a common mistake: patients say “I’m allergic to morphine” when they just threw up. That’s not an allergy. That’s a side effect. But if you say “allergic,” the team might avoid all opioids - even ones that won’t cause the same issue. Instead, be specific:- “I had hives and swelling after receiving rocuronium during my last surgery.”
- “I got severe nausea and vomiting after codeine - I couldn’t keep anything down for 12 hours.”
- “I broke out in a rash after taking ibuprofen - it lasted three days.”

What Your Medical Team Needs to Know
Your care team isn’t just looking for “allergies.” They need a full picture:- Drug names: Generic and brand names matter. “Succinylcholine” and “Anectine” are the same - but if you only remember “the shot they gave me for intubation,” that’s okay - just describe it.
- Reaction timing: Did symptoms start during the procedure? Within 30 minutes? Hours later?
- Severity: Did you need epinephrine? Were you admitted to the ICU? Did you nearly die?
- Treatment: What helped? Did steroids or antihistamines calm it down?
- Other meds: Are you on blood thinners? Antidepressants? Diabetes meds? These can interact with anesthesia.
What to Do If You’ve Never Been Asked
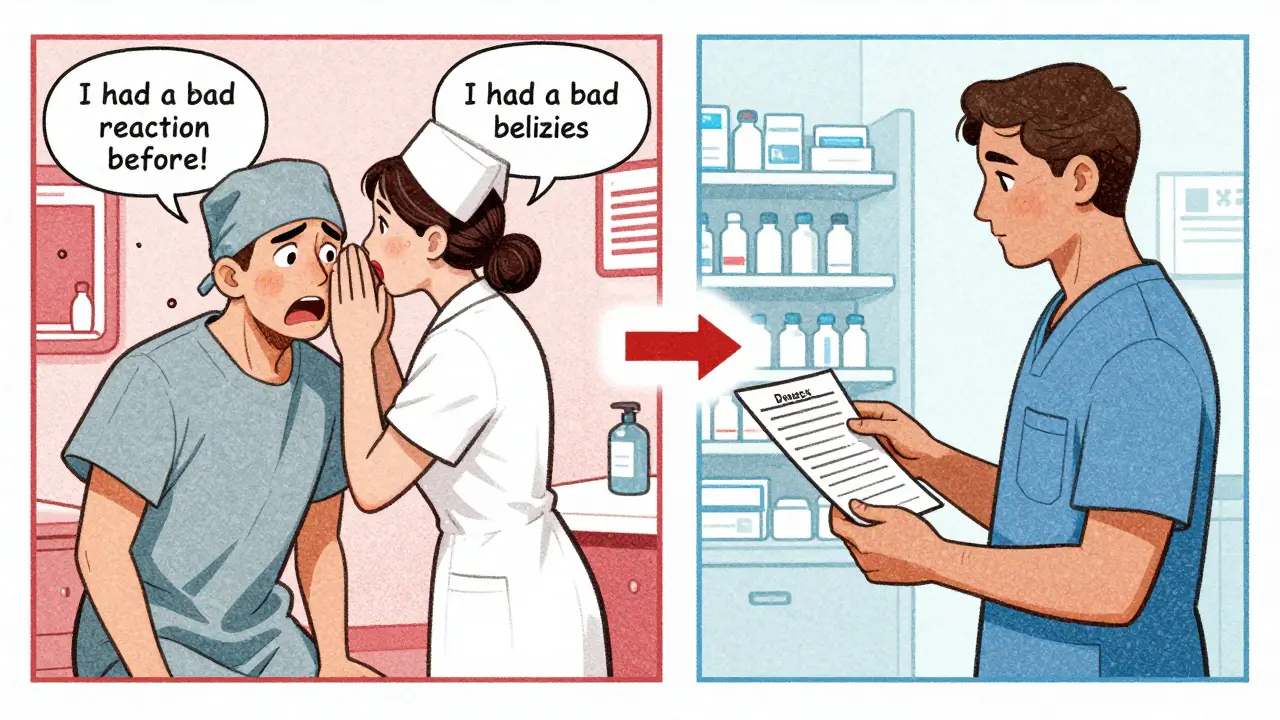
You’d think this would be automatic. But a 2023 survey found that 38% of patients who had a reaction weren’t given clear documentation afterward. And 37% of emergency surgeries still have incomplete allergy records. If you’re being rushed - and you’ve had a reaction before - speak up. Say:“I’ve had a serious reaction to a drug before. I need to make sure this is documented and reviewed before we start.”
You have the right to ask for a pharmacist to review your medications. You have the right to ask for an anesthesiologist to talk to you personally before surgery. You have the right to ask for a delay if you need more time to get your history in order. Don’t be polite. Be firm. This isn’t about being difficult - it’s about survival.Special Cases: High-Risk Drugs and Timing
Some drugs need to be stopped days before surgery. If you’re on any of these, you need to know:- NSAIDs (ibuprofen, naproxen): Stop 7 days before surgery. Some doctors allow 5 days if you’re low-risk.
- Prasugrel (Effient): Must be stopped 7 days before.
- Ticagrelor (Brilinta): Stop 3-5 days before.
- MAO inhibitors (antidepressants like phenelzine): Must be stopped 2 weeks before. Certain anesthetics like ephedrine or meperidine can cause deadly spikes in blood pressure.
Get a Physical Allergy Card
Most allergists recommend carrying a wallet-sized allergy card. You can make one for free at the American Academy of Allergy, Asthma & Immunology’s website. List:- Drug names you react to
- Reaction type (e.g., “anaphylaxis,” “severe nausea”)
- Alternative drugs that are safe
- Your contact info
What Happens After Your Surgery?
If you had a reaction during surgery - even if it was mild - you need follow-up. The Spanish Journal of Anesthesia and Critical Care recommends you see an allergist within 4-6 weeks. Why? Because:- You might need testing to confirm what caused it.
- You might need an epinephrine auto-injector.
- You’ll get a formal diagnosis that can be added to your records.
Real Stories - What Went Right and Wrong
One patient on Reddit shared: “I had a reaction to rocuronium 10 years ago. The pre-op nurse spent 20 minutes writing everything down - even what I ate that day. I felt heard.” Another patient on Healthgrades wrote: “They ignored my codeine allergy. I was sick for days after surgery.” The difference? Documentation. One person was treated like a person. The other was treated like a checkbox.Final Checklist Before Surgery
Use this before your pre-op appointment:- ✅ List all medications you’ve taken in the last 6 months (including supplements)
- ✅ Write down every reaction you’ve ever had - no matter how small
- ✅ Bring old medical records or allergy cards
- ✅ Know the names of any drugs you reacted to (or describe them)
- ✅ Ask: “Will a pharmacist review my meds before surgery?”
- ✅ Ask: “Will the anesthesiologist talk to me directly?”
- ✅ Ask: “Can I get a copy of my allergy documentation?”
What if I don’t remember the name of the drug I reacted to?
It’s okay. Describe the drug - what it looked like, when you took it, what it was for. Say, “It was a blue pill I took after surgery,” or “It was an IV given during my last procedure.” Even vague details help your team rule out options. They’ll cross-reference it with your medical history.
Can I be tested to confirm a drug allergy?
Yes - especially if you’ve had a serious reaction like anaphylaxis, swelling, or breathing trouble. Allergists can do skin tests or blood tests to confirm if it’s a true allergy. You should see one within 4-8 weeks after the reaction. Many hospitals have referral programs for this.
What if I’m having emergency surgery and haven’t told anyone about my reaction?
Tell whoever is closest to you - the nurse, the paramedic, your family member. Say, “I’ve had a bad reaction to medicine before.” Even if you don’t know the name, the team will avoid drugs that commonly cause reactions. Emergency teams are trained to use safer alternatives if they don’t know your history. But the more you say, the better.
Do I need to tell my dentist or other doctors about my drug reactions too?
Yes. Drug reactions don’t just matter for surgery. They matter for antibiotics, painkillers, dental procedures, and even MRIs (which use contrast dyes). Always update every provider you see. Keep your allergy card handy.
Are herbal supplements and vitamins really a concern?
Absolutely. St. John’s Wort can interfere with anesthesia. Garlic and ginkgo can thin your blood. Fish oil can increase bleeding risk. Even vitamin E and ginseng have been linked to complications. List every supplement you take - no matter how “natural” it seems.


Juan Reibelo
Okay, I’ve had two surgeries, and honestly? I thought saying ‘I’m allergic to penicillin’ was enough. Turns out, I had a rash from amoxicillin-no anaphylaxis, no breathing issues. But the anesthesiologist asked for details, and I panicked. Now I keep a note on my phone: ‘Rash + itching after amoxicillin, 2018. Not anaphylaxis.’ I wish I’d known this years ago.