Recovering from opioid addiction feels like navigating a maze where every turn can trigger old habits. While medication and counseling form the backbone of treatment, self-care provides the daily fuel that keeps you moving forward. When you make time for simple, intentional habits-like a short walk, a balanced meal, or a breath‑focused pause-you give your brain and body the chance to heal, reducing cravings and building confidence.
Key Takeaways
- Self‑care strengthens the brain’s reward system, making cravings less powerful.
- Physical activity, nutrition, sleep, and mindfulness each address a different relapse trigger.
- Consistent habits create a sense of control that combats feelings of helplessness.
- Support networks amplify self‑care benefits by providing accountability.
- Tracking progress with simple tools helps you notice improvement before setbacks appear.
Self‑care is a set of intentional actions that promote physical, emotional, and social wellbeing. In the context of opioid recovery, it means choosing activities that restore balance and reduce stress, rather than turning to substances for relief. While treatment programs address the medical side of addiction, self‑care fills the everyday gaps that keep you steady when you’re outside a clinic.
Opioid addiction is a chronic brain disorder characterized by compulsive drug‑seeking behavior despite harmful consequences. The powerful neurochemical changes created by opioids alter pain perception, reward pathways, and stress response, making recovery a multifaceted challenge.
Recovery refers to the ongoing process of maintaining sobriety, improving health, and rebuilding a fulfilling life. It is not a single event but a series of daily choices that reinforce new, healthier patterns. Among those choices, self‑care is the most accessible and immediate.
How Self‑Care Supports the Brain’s Recovery
When you engage in regular self‑care, you stimulate the brain’s natural dopamine production without drugs. Activities like exercise, listening to music, or cooking a nutritious meal trigger the reward system in a safe way, gradually re‑training the brain to seek pleasure from healthy sources.
Research from the National Institute on Drug Abuse (2024) shows that patients who incorporated daily physical activity experienced a 30% reduction in cravings compared with those who did not. The same study noted lower anxiety scores, which are often the hidden drivers of relapse.
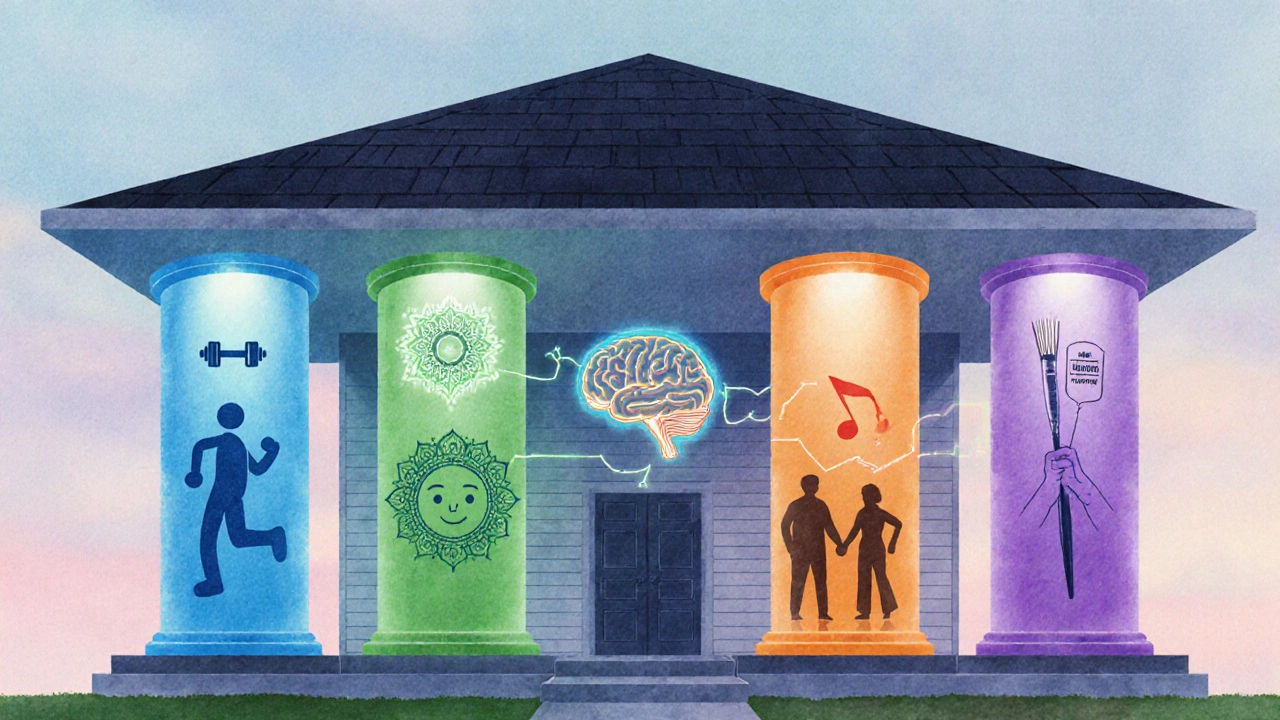
Four Pillars of Self‑Care for Opioid Recovery
Think of self‑care as a house built on four sturdy pillars. Neglect one, and the structure feels shaky.
- Physical Health: Exercise, balanced nutrition, and proper sleep.
- Emotional Health: Mindfulness, journaling, and therapy.
- Social Connection: Support groups, family time, and community activities.
- Spiritual/Meaningful Activities: Hobbies, volunteering, or any practice that gives purpose.
Practical Daily Habits
Below is a quick‑reference checklist you can print or keep on your phone. Choose one item from each column each day, and watch how it adds up.
| Self‑Care Area | Action | Approx. Time |
|---|---|---|
| Physical | 30‑minute brisk walk or jog | 30min |
| Nutrition | Prepare a protein‑rich meal with veggies | 45min |
| Sleep | Set a regular bedtime, limit screens 1hour before | 8hr |
| Emotional | Mindfulness meditation for 10minutes | 10min |
| Social | Call a friend or attend a support group | 20min |
| Spiritual | Spend 15minutes on a hobby you love | 15min |
Managing Cravings and Triggers
Cravings often spike when stress, boredom, or anger hit. By having a self‑care toolbox ready, you can pivot quickly. For example, if you feel a sudden urge after a stressful work call, a 5‑minute breath‑focused exercise (a form of Mindfulness practice) can calm the nervous system enough to choose a healthier response.
Another effective tactic is “the 30‑minute rule.” When a craving appears, commit to a non‑substance activity for the next 30minutes-walk, call a sponsor, or write in a journal. Most cravings lose intensity within that window.
Building a Support Network
Support groups provide a safe space to share setbacks and celebrate victories. They also expose you to peers who understand the daily battle, offering tips that fit real life.
Working with a qualified Therapist or counselor adds a professional layer of accountability. Therapists can teach coping skills, such as cognitive‑behavioral strategies, that complement self‑care routines.
Setting Realistic Goals and Tracking Progress
Goal‑setting works best when it’s specific, measurable, attainable, relevant, and time‑bound (SMART). Instead of “I’ll be healthier,” try “I’ll walk 10,000 steps three times a week for the next month.” Write the goal in a journal or a phone app, and note any obstacles you face.
Tracking creates visible proof of improvement, which boosts motivation. Even tiny wins-like choosing water over soda-add up and make larger challenges feel less daunting.

Common Pitfalls and How to Avoid Them
1. Thinking self‑care is optional. In reality, it’s a core component of recovery. Treat it like medication-schedule it, and don’t skip without a reason.
2. Trying to overhaul everything at once. Start with one habit, solidify it for two weeks, then add another. Gradual change prevents overwhelm.
3. Neglecting pleasure. Recovery isn’t about deprivation. Include activities that genuinely bring joy-whether it’s gardening, painting, or a favorite TV show.
4. Isolating yourself. Even introverts need some connection. A brief text check‑in or a weekly group call keeps loneliness at bay.
Next Steps: Your Personal Self‑Care Action Plan
- Pick three items from the Daily Checklist you feel confident about.
- Write them on a sticky note and place it where you’ll see it each morning.
- Schedule a 15‑minute call with a friend or sponsor for the coming week.
- Set a reminder to log your mood and cravings in a journal each night.
- Review your notes weekly; adjust any habits that feel too hard or not helpful.
Frequently Asked Questions
Can self‑care replace medication‑assisted treatment?
No. Medication‑assisted treatment (MAT) addresses the physiological cravings, while self‑care tackles everyday stressors and emotional wellbeing. Both work best together.
How much exercise is enough for someone in early recovery?
Start with 10‑15 minutes of low‑impact activity, like walking or stretching, and gradually increase to 30 minutes most days of the week. Consistency matters more than intensity.
What if I miss a self‑care habit for a day?
Missing a day isn’t a failure; it’s a data point. Note why it happened, then get back on track the next day. The goal is long‑term consistency, not perfection.
Is mindfulness the same as meditation?
Mindfulness is the broader practice of staying present, which can be applied in daily activities. Meditation is a formal, seated version of mindfulness that often lasts 5‑30 minutes.
How can I involve my family without feeling judged?
Share a brief update about your recovery goals and ask for specific support, like joining you for a walk or listening without offering unsolicited advice.


Matt Cress
Wow, self‑care, never heard of that in rehab, right?