When your muscles suddenly feel heavy, your stairs become a mountain, and even lifting a coffee cup feels like a workout, it’s easy to blame aging or laziness. But if this weakness comes with a purple rash on your eyelids or trouble swallowing, it might not be fatigue-it could be dermatomyositis or polymyositis. These are rare autoimmune diseases where your immune system turns on your own muscles, causing chronic inflammation and progressive weakness. Unlike a pulled muscle or overtraining, this damage doesn’t heal with rest. It needs precise diagnosis and aggressive treatment-before permanent damage sets in.
What Sets Dermatomyositis Apart from Polymyositis?
Both conditions attack the same muscle groups-hips, thighs, shoulders, and neck-but dermatomyositis has a visible signature: skin changes. The hallmark is the heliotrope rash, a violet or reddish-purple discoloration on the upper eyelids. You’ll also see red, scaly patches over knuckles, elbows, knees, or the V of the neck. These aren’t just cosmetic. They’re a red flag that your immune system is in overdrive.
Polymyositis doesn’t touch the skin. Its only sign is symmetrical muscle weakness. You might notice you can’t get up from a chair without using your arms, or your hairbrush feels too heavy to lift. The weakness creeps in slowly, often over weeks or months, and affects both sides of your body equally. That’s why it’s often mistaken for fibromyalgia, thyroid issues, or even normal aging.
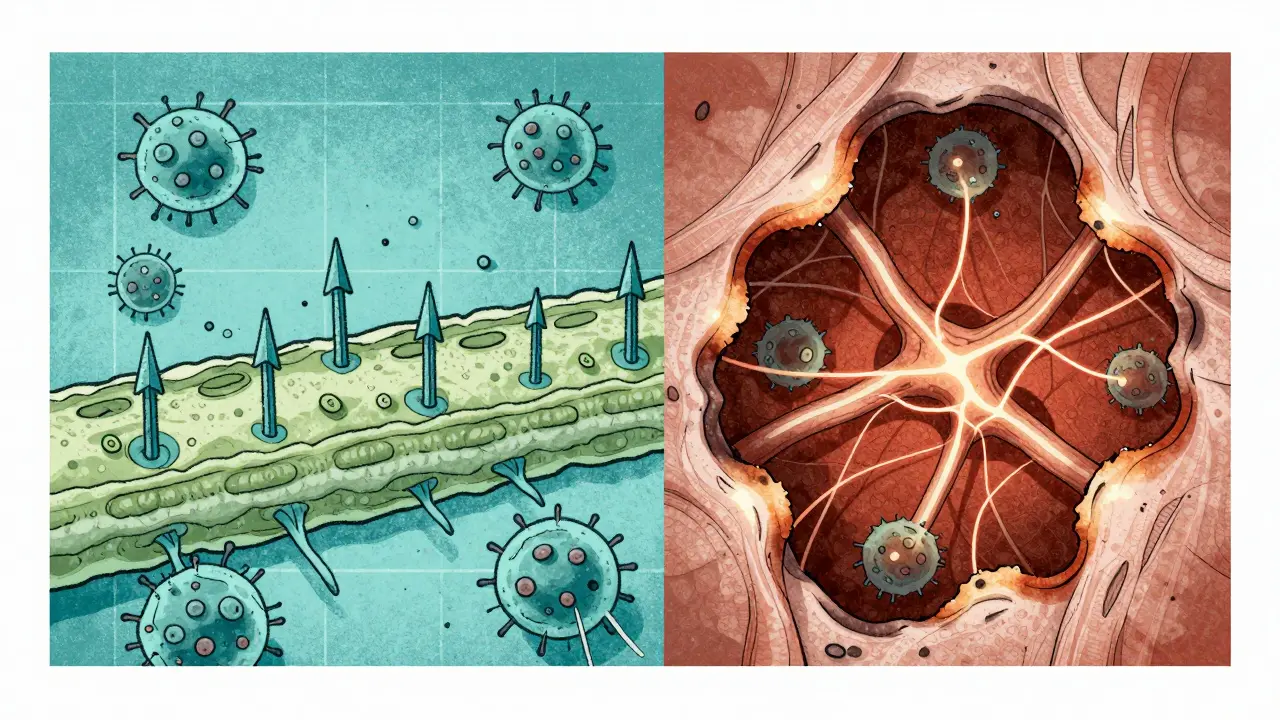
The real difference lies beneath the surface. In dermatomyositis, antibodies and B cells attack blood vessels feeding muscle tissue, leading to perifascicular atrophy-where muscle fibers around the edges of bundles waste away. In polymyositis, T cells invade and destroy muscle fibers directly. This distinction matters because it affects how the disease responds to treatment.
How Is It Diagnosed?
There’s no single blood test that confirms either condition. Diagnosis is a puzzle solved with multiple pieces:
- Blood tests show elevated creatine phosphokinase (CPK), often 5 to 10 times higher than normal (normal range: 10-120 U/L). Other markers like aldolase, ESR, and CRP also rise with inflammation.
- Electromyography (EMG) detects abnormal electrical activity in muscles-short, low-amplitude bursts and spontaneous firing that signal damaged fibers.
- MRI scans reveal swelling and inflammation in specific muscle groups, helping doctors pick the best spot for biopsy.
- Muscle biopsy is the gold standard. In polymyositis, you’ll see T cells clustered around non-dead muscle fibers. In dermatomyositis, the pattern is different: damaged fibers at the edges of muscle bundles and immune cells around small blood vessels.
Doctors also test for myositis-specific antibodies (MSAs), like anti-Jo-1 or anti-Mi-2. These aren’t just diagnostic-they help predict complications. For example, anti-synthetase antibodies often come with lung disease, while anti-MDA5 antibodies in dermatomyositis signal a higher risk of severe skin ulcers and lung scarring.
One critical step: cancer screening. About 20% of adults with dermatomyositis have an underlying cancer-often ovarian, lung, or colon cancer. That’s why a new diagnosis triggers mammograms, colonoscopies, pelvic ultrasounds, and chest CT scans. Polymyositis doesn’t carry that same cancer link.
Why Diagnosis Takes So Long
It’s not unusual to wait over two years for a correct diagnosis. Many patients see four or more doctors before someone recognizes the pattern. Why? Because the symptoms mimic other conditions. Fatigue and muscle aches? Could be chronic fatigue syndrome. Skin rash? Maybe eczema or lupus. Trouble swallowing? Could be GERD or a neurological issue.
A 2022 survey of 1,247 patients found that 30% were initially misdiagnosed. One woman in London spent 18 months being treated for “stress-related muscle tension” before a rheumatologist spotted the heliotrope rash and ordered a biopsy. Another man thought his weakness was from sitting too much at his desk job-until he couldn’t climb stairs without holding the railing.
Delayed diagnosis means more muscle damage. The longer inflammation goes unchecked, the more muscle turns to scar tissue. That’s why early treatment is non-negotiable. Studies show patients who start treatment within six months of symptom onset have an 80% chance of reaching low disease activity or remission.
First-Line Treatment: Steroids and Their Costs
Prednisone is the starting point for both conditions. Doctors typically begin with 1 mg per kilogram of body weight daily-about 40 to 60 mg for most adults. Within weeks, many patients notice improved strength. But steroids are a double-edged sword.
Long-term use brings serious side effects:
- 30-50% of patients develop osteoporosis
- 15-30% develop steroid-induced diabetes
- 20-40% get cataracts
- 82% report significant weight gain
- 67% struggle with insomnia
That’s why doctors don’t keep you on high doses forever. After 4-8 weeks, they start tapering slowly-often over months or even years. To protect bones, patients get calcium, vitamin D, and sometimes bisphosphonates. Blood sugar and eye exams are monitored regularly.
Second-Line Drugs: When Steroids Aren’t Enough
Half of patients don’t respond well to steroids alone. That’s when second-line drugs kick in:
- Methotrexate is the most common. It’s taken weekly, and many patients see CK levels drop by 50% within 3-4 months.
- Azathioprine and mycophenolate mofetil are alternatives, especially for those who can’t tolerate methotrexate.
- Intravenous immunoglobulin (IVIG) is especially helpful for dermatomyositis with severe skin disease or swallowing problems. It works by calming the immune system with donated antibodies.
- Rituximab, a drug originally for lymphoma, has shown 60-70% response rates in refractory cases. It’s used off-label but backed by solid trial data.
One patient from Manchester shared on Reddit: “After nine months of prednisone with no improvement, I started methotrexate. My CPK dropped from 8,200 to 450 in four months. I cut my steroid dose from 40 mg to 10 mg.”
New Hope: JAK Inhibitors and Biologics
Recent trials are changing the game. In 2023, the IMACS trial showed that tofacitinib, a JAK inhibitor used for rheumatoid arthritis, improved skin rashes by 65% and muscle strength by 52% in dermatomyositis patients after 24 weeks. Another drug, abatacept, is being tested in polymyositis and has shown promise in early trials.
These drugs target specific parts of the immune system, offering more precision than broad immunosuppressants. They’re not yet FDA-approved for myositis, but many rheumatologists are prescribing them off-label for stubborn cases.
Physical Therapy: The Hidden Lifesaver
Medications stop the attack-but exercise rebuilds what’s lost. Physical therapy isn’t optional. It’s essential. A 2022 report from the Hospital for Special Surgery found that patients who stuck with a tailored exercise program improved their functional capacity by 35-45% in six months.
Therapy starts with low-resistance movements: leg lifts, seated marches, wall push-ups. The goal isn’t to build muscle-it’s to prevent atrophy and keep joints mobile. Too much strain can worsen inflammation, so therapists avoid high weights or intense cardio.
Patients who skip therapy often end up permanently weak. One woman in her 50s said, “I thought rest was healing. I didn’t move for months. By the time I started PT, I needed a walker.”
Managing Complications: Lungs, Swallowing, and More
Interstitial lung disease affects 30-40% of dermatomyositis patients. It causes scarring in the lungs, leading to shortness of breath and dry cough. Regular pulmonary function tests and high-resolution CT scans are part of routine monitoring.
Dysphagia-trouble swallowing-is common in both conditions. It can lead to choking or aspiration pneumonia. Speech therapists help with swallowing exercises and recommend softer foods or thickened liquids.
Calcium and vitamin D supplements are standard. Bone density scans are done yearly. Eye exams every 6-12 months catch cataracts early.
Prognosis: Better Than Ever
Thirty years ago, 10-year survival rates for these diseases were below 60%. Today, they’re over 80% for dermatomyositis and 85% for polymyositis. Why? Earlier diagnosis, better drugs, and multidisciplinary care.
Patients who respond well to treatment can live full lives. Many return to work, drive, and care for their families. But it’s a marathon, not a sprint. Relapses happen. Medications need adjusting. Side effects must be managed.
What Patients Wish They Knew Sooner
From hundreds of patient forums and surveys, three themes stand out:
- Don’t wait for the rash to disappear. If you have muscle weakness, get tested-even if the rash fades.
- Find a rheumatologist who specializes in myositis. General rheumatologists may not know the latest protocols. Look for centers with myositis clinics.
- Join a support group. The Myositis Support and Understanding Association and The Myositis Association offer resources, webinars, and peer connections. You’re not alone.
One man in London said, “I thought I was dying. Then I found a group of people who knew exactly what I was going through. That gave me hope I didn’t know I needed.”
Where the System Falls Short
Even with better outcomes, access is unequal. In the U.S., 40% of patients face delays in getting second-line drugs due to insurance prior authorizations-averaging 17 days per request. In the UK, NHS wait times for specialist referrals can stretch beyond three months.
There are only about 5,800 rheumatologists in the U.S. for 58 million people with autoimmune diseases. That’s one specialist for every 10,000 patients. Many areas have none.
Drug development is slow. Only three drugs are approved for dermatomyositis-none for polymyositis. Most treatments are used off-label, meaning insurance may deny coverage.
Research funding is minimal. Only 15% of rare autoimmune disease trials focus on myositis. More investment could bring faster answers.
What You Can Do Today
If you or someone you know has unexplained muscle weakness:
- See your doctor and ask for a CPK blood test.
- Take photos of any rashes-especially on eyelids or knuckles.
- Write down when symptoms started and what makes them better or worse.
- Request a referral to a rheumatologist if weakness lasts more than four weeks.
- Don’t delay. Early treatment saves muscle-and your future.
These diseases don’t vanish. But with the right care, they can be controlled. You don’t have to lose your strength. You don’t have to live in fear. Help is out there-you just need to start asking the right questions.
Is dermatomyositis the same as polymyositis?
No. Both cause muscle inflammation and weakness, but dermatomyositis includes distinctive skin rashes-like a purple eyelid rash-and is linked to a higher risk of cancer and lung disease. Polymyositis affects only muscles and doesn’t involve the skin. Their underlying immune mechanisms are also different: dermatomyositis is driven by antibodies, while polymyositis involves direct T-cell attacks on muscle fibers.
Can you cure dermatomyositis or polymyositis?
There is no cure yet. But with early, aggressive treatment, most patients achieve remission or low disease activity. Many regain near-normal strength and function. The goal is to suppress the immune attack, prevent muscle damage, and manage side effects long-term.
How long does it take to get diagnosed?
On average, it takes 2 to 3 years. Many patients see multiple doctors before a specialist recognizes the pattern. Delays happen because symptoms mimic more common conditions like fibromyalgia, thyroid disease, or aging. Early signs like a heliotrope rash or rising CPK levels should trigger urgent referral to a rheumatologist.
Are steroids the only treatment option?
No. Steroids like prednisone are the first step, but they’re not enough for many patients. Second-line drugs like methotrexate, azathioprine, mycophenolate, IVIG, and rituximab are commonly used. Newer drugs like JAK inhibitors (tofacitinib) are showing strong results in clinical trials and are increasingly used off-label for resistant cases.
Does physical therapy really help?
Yes. Studies show that structured, low-resistance physical therapy improves muscle strength and function by 35-45% within six months. It prevents muscle wasting and joint stiffness. Without it, even patients who respond to medication can end up permanently weak. Therapy should start within two weeks of diagnosis.
Why is cancer screening important for dermatomyositis?
About 20% of adults diagnosed with dermatomyositis have an underlying cancer-often ovarian, lung, or gastrointestinal. The immune system’s attack on muscle may be triggered by cancer cells. Screening at diagnosis (mammograms, colonoscopies, pelvic ultrasounds, CT scans) can catch cancer early, improving survival for both the cancer and the myositis.
Can children get dermatomyositis or polymyositis?
Dermatomyositis can occur in children, typically between ages 5 and 15. It’s called juvenile dermatomyositis and has slightly different features, like calcium deposits under the skin. Polymyositis, however, is extremely rare in children and is almost exclusively an adult disease. Pediatric cases require specialized care.
What are the biggest side effects of long-term steroid use?
The most common are weight gain (82% of patients), osteoporosis (30-50%), diabetes (15-30%), cataracts (20-40%), insomnia (67%), and mood changes. Doctors counter these with calcium/vitamin D, bone density scans, blood sugar monitoring, eye exams, and gradual steroid tapering. Never stop steroids suddenly-this can be life-threatening.


Mario Bros
I was diagnosed with dermatomyositis last year and honestly? This post nailed it. Started on prednisone and felt like a balloon with legs. Now on methotrexate and my CPK dropped from 9k to 500. PT saved my life. 💪