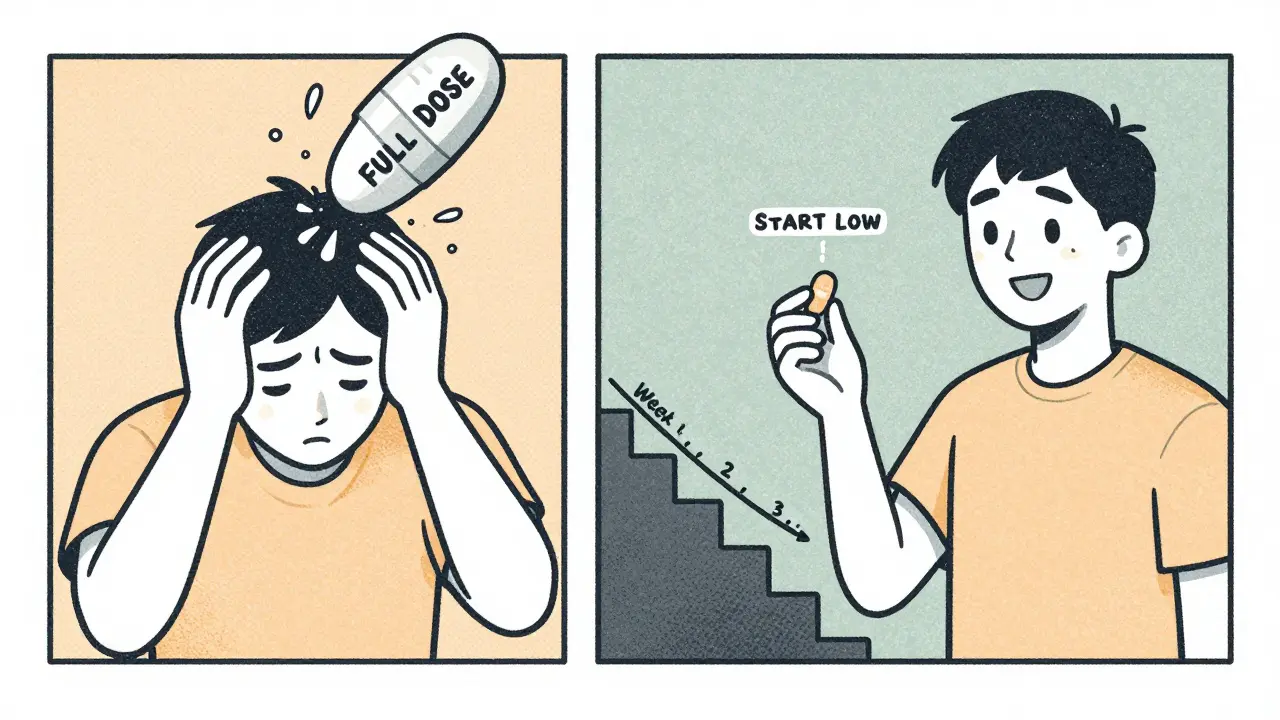
When you start a new medication, it’s not about taking the highest dose right away. It’s about finding the lowest dose that still works - without making you feel awful. That’s where dose titration comes in. It’s not a fancy term for doctors to sound smart. It’s a simple, proven method to help you get the benefits of a drug without the nausea, dizziness, anxiety, or worse. And if you’ve ever been put on a medication that made you feel worse before it helped, you’ve probably seen what happens when titration is skipped.
Think of it like turning up a dimmer switch instead of flipping a light switch all the way on. Some medications, especially those for mental health, epilepsy, or heart conditions, have a very narrow window between helping you and hurting you. Too little, and nothing changes. Too much, and you’re stuck in bed with side effects that feel worse than the original problem. Dose titration is the process of slowly adjusting that dose, step by step, to find your personal sweet spot.
How Dose Titration Actually Works
It starts with a low dose - often 25% to 50% of the final target. For example, if the usual dose of a stimulant for ADHD is 20mg, you might start at 5mg. You take it for a few days to a week, then your doctor checks in. Did you feel jittery? Sleep better? Get headaches? Based on that, they might increase it by 2.5mg or 5mg. Then you wait again. This isn’t guesswork. It’s science built on decades of clinical data.
For stimulants like Adderall or Vyvanse, this usually takes 4 to 6 weeks. For non-stimulants like atomoxetine, it can stretch to 8 to 12 weeks. Why? Because some drugs hit your system fast. Others build up slowly in your bloodstream. Rushing it doesn’t speed up results - it just increases the chance of side effects.
Take venetoclax, a drug used for leukemia. If you started at the full 400mg dose, you’d risk tumor lysis syndrome - a dangerous condition where dying cancer cells flood your blood with toxins. But if you start at 20mg and increase weekly, your body has time to adjust. That’s not optional. It’s built into the FDA-approved labeling. Same with lamotrigine for epilepsy. Jumping straight to 100mg could trigger a life-threatening skin reaction. Titration reduces that risk by over 90%.
Why Some Medications Need It More Than Others
Not all drugs need careful titration. Some, like ibuprofen or acetaminophen, have wide safety margins. You can take a little more without crashing. But others? Not so much.
Warfarin, for example, is a blood thinner with a very tight window. The goal is to keep your INR between 2.0 and 3.0. Go below, and you risk clots. Go above, and you risk bleeding. Studies show 67% of patients on warfarin need at least one dose change in the first month. Compare that to apixaban, a newer blood thinner - only 28% need adjustments. Why? Because apixaban’s effects are more predictable. Warfarin? It reacts with food, other meds, even your liver enzymes. That’s why weekly blood tests and slow titration are standard.
Same with thyroid meds. Levothyroxine for hypothyroidism often starts at 25mcg, then increases by 12.5 to 25mcg every 4 to 6 weeks. Too fast, and you get heart palpitations. Too slow, and fatigue drags on. But liothyronine? It acts faster and is harder to titrate - which is why it’s not usually the first choice.
The bottom line? The narrower the therapeutic index - the closer the effective dose is to the toxic one - the more critical titration becomes. That’s why 87% of medications with precise dosing requirements now include titration instructions on their FDA labels.
What Happens When Titration Is Ignored
Skipping titration isn’t just a mistake - it’s common. And it’s why so many people quit their meds.
A 2022 survey of 1,200 ADHD patients found that 74% who followed a slow titration plan reported manageable side effects. Only 41% of those who started at full dose did. One Reddit user wrote: “My doctor started me on 10mg Adderall. I couldn’t sleep, my heart raced, I cried for no reason. I quit for two years. Then I found a doctor who started me at 5mg. Now I’m stable.” That’s not an outlier. It’s a pattern.
Doctors sometimes skip titration because they’re rushed. Or because they assume “everyone reacts the same.” But people don’t. Your metabolism, your liver enzymes, your weight, your other meds - they all change how your body handles a drug. A dose that’s perfect for one person could be too much for another.
And it’s not just mental health. Beta-blockers for heart failure? A 2022 American Heart Association study found that gradual up-titration cut the rate of patients quitting due to side effects from 45% down to 18%. That’s a massive difference - all from taking it slow.
How to Make Titration Work for You
If you’re starting a new medication that requires titration, here’s how to make it work:
- Keep a side effect journal. Note the time you take the pill, what you ate, your mood, sleep, energy, and any physical symptoms. Use a 1-10 scale. A 2023 Healthgrades review found that 78% of people who tracked symptoms had better outcomes.
- Wait at least a week between dose changes. Side effects can lag. A headache on day 2 might not be from the new dose - it might be from stress or dehydration. Give your body time to adjust.
- Take meds with food if recommended. Many drugs cause stomach upset. Taking them with a light snack can cut that risk by 65%, according to user reports on Drugs.com.
- Ask for a written titration plan. Some meds, like Vyvanse, come with detailed guides. Others? Not so much. If your doctor doesn’t give you one, ask. A clear schedule reduces anxiety and improves adherence.
- Don’t skip appointments. Weekly check-ins during titration aren’t optional. They’re how your doctor spots patterns you might miss.
It’s not just about following instructions. It’s about communication. If you feel worse, say so. If you feel nothing, say so. Your input is part of the process.
The Future of Personalized Titration
This isn’t just about trial and error anymore. Technology is stepping in.
In January 2023, the FDA cleared the TitrationTracker app - the first AI-powered tool designed to predict the best next dose based on your daily symptom logs. A March 2023 study in Nature Digital Medicine showed it reduced side effects by 32% compared to standard care.
Even more promising? Pharmacogenetic testing. Your genes can tell doctors how fast you metabolize certain drugs. Right now, 28 medications - including some antidepressants and blood thinners - have genetic guidelines. By 2025, that number will grow to 40. The American College of Clinical Pharmacology predicts that by 2030, 75% of high-risk medications will use genetic data to set starting doses.
Imagine starting your ADHD medication not at 5mg, but at 2.5mg because your genes say you process it slowly. Or avoiding a drug entirely because your liver can’t handle it. That’s not sci-fi. It’s coming.

Where Titration Falls Short
It’s not a magic fix. Titration doesn’t work in emergencies. If you’re having a seizure or a heart attack, you need the full dose now. No waiting.
It also doesn’t work well in places with limited healthcare access. In low-income countries, only 22% have standardized titration protocols, according to the WHO. Weekly check-ins? Blood tests? They’re not always possible. That’s why global health efforts are pushing for simpler, longer-acting formulations.
And yes - it takes time. Eight to twelve weeks. That’s longer than most people expect. It’s easy to get frustrated. “Why am I still tired after 3 weeks?” you might ask. But that’s the point. You’re not supposed to feel great right away. You’re supposed to feel better without feeling awful.
The real win? A 2021 meta-analysis found titration reduces initial side effects by 40% to 60%. That’s not small. That’s life-changing.
Final Thoughts
Dose titration isn’t about being careful. It’s about being smart. It’s about respecting your body’s limits while giving the medicine time to work. The goal isn’t to get to the highest dose. It’s to get to the right dose - the one that lets you live your life without side effects holding you back.
Don’t be afraid to ask for it. Don’t be pressured into a full dose on day one. And don’t give up if the first few weeks feel slow. The science is clear: starting low and going slow is the most effective way to reduce side effects - and stick with the treatment that can help you.

