Allergic Reaction Severity Calculator
When you take a new medication, you expect relief - not a rash, swelling, or trouble breathing. But for millions of people, even common drugs like penicillin, ibuprofen, or sulfa antibiotics can trigger an allergic reaction. The problem? Not all reactions are the same. Some are annoying. Others are life-threatening. And most people can’t tell the difference until it’s too late.
Let’s cut through the confusion. This isn’t about medical jargon. It’s about knowing what to look for, when to act, and why timing matters more than you think.
What Actually Counts as an Allergic Reaction?
Not every side effect is an allergy. If you get a stomachache after taking aspirin, that’s not an allergy - it’s a side effect. True drug allergies happen when your immune system mistakes the medicine for a threat. It’s like your body’s alarm system going off for no reason. Once that happens, your body remembers. Next time you take the same drug, the reaction can be faster and worse.
According to research, about 7 to 10% of people have some kind of drug allergy. Antibiotics - especially penicillin - top the list. But NSAIDs like ibuprofen and naproxen, chemotherapy drugs, and anticonvulsants like carbamazepine also trigger reactions often. The real danger? Many people think they’re allergic when they’re not. Studies show up to 80% of people who say they’re allergic to penicillin test negative when checked properly. That means they’re avoiding safe, effective drugs unnecessarily.
Mild Reactions: The Red Flag You Might Ignore
Mild reactions are common. They’re also the most misunderstood.
You might notice a few red, itchy spots on your arms or chest - that’s hives. Or maybe your skin feels warm and flushed. A small rash on your neck after taking a new antibiotic? You might brush it off as "just a reaction." But here’s the truth: mild doesn’t mean harmless.
These reactions are usually Type I (IgE-mediated) or Type IV (T-cell mediated). Type I hits fast - within minutes to an hour. Histamine levels rise to 2-5 ng/mL. You get localized hives covering less than 10% of your skin. Itchy eyes? A runny nose? These can be signs too.
What to do? Stop the drug. Take an over-the-counter antihistamine like cetirizine or loratadine. Symptoms usually fade in 24 to 48 hours. But here’s the catch: if this is your first reaction, don’t assume it’ll stay mild. Next time, it could be worse.
One Reddit user shared: "Took amoxicillin. Got a few hives. Didn’t think much of it. Two weeks later, same drug - ended up in the ER with swelling all over." That’s not rare. Mild reactions are often the warning shot before a bigger one.
Moderate Reactions: The System Is Starting to Fail
Moderate reactions are where things get serious - fast.
Instead of a few spots, you’re covered in hives across 10-30% of your body. Your lips or eyelids swell. You feel dizzy. Your temperature spikes to 38.5°C or higher. Maybe your throat feels tight. You’re not gasping for air yet - but you’re not fine either.
This is where the immune system is no longer just reacting locally. Histamine levels climb to 5-10 ng/mL. You might develop angioedema (deep swelling under the skin), or symptoms of serum sickness: fever, swollen lymph nodes, joint pain. These often happen 7-14 days after taking a drug, especially antibiotics or antiseizure meds.
These reactions need more than antihistamines. You’ll likely need corticosteroids - either oral or injected - to calm the immune response. And you need to be monitored. A 2024 study from Langford Allergy found that 75% of moderate NSAID reactions resolve within 72 hours with treatment. But if you wait too long? It can spiral.
Don’t go home and wait it out. Go to urgent care. Or call your doctor. If you’re not seen within a few hours, you risk slipping into severe territory.

Severe Reactions: The Emergency You Can’t Afford to Miss
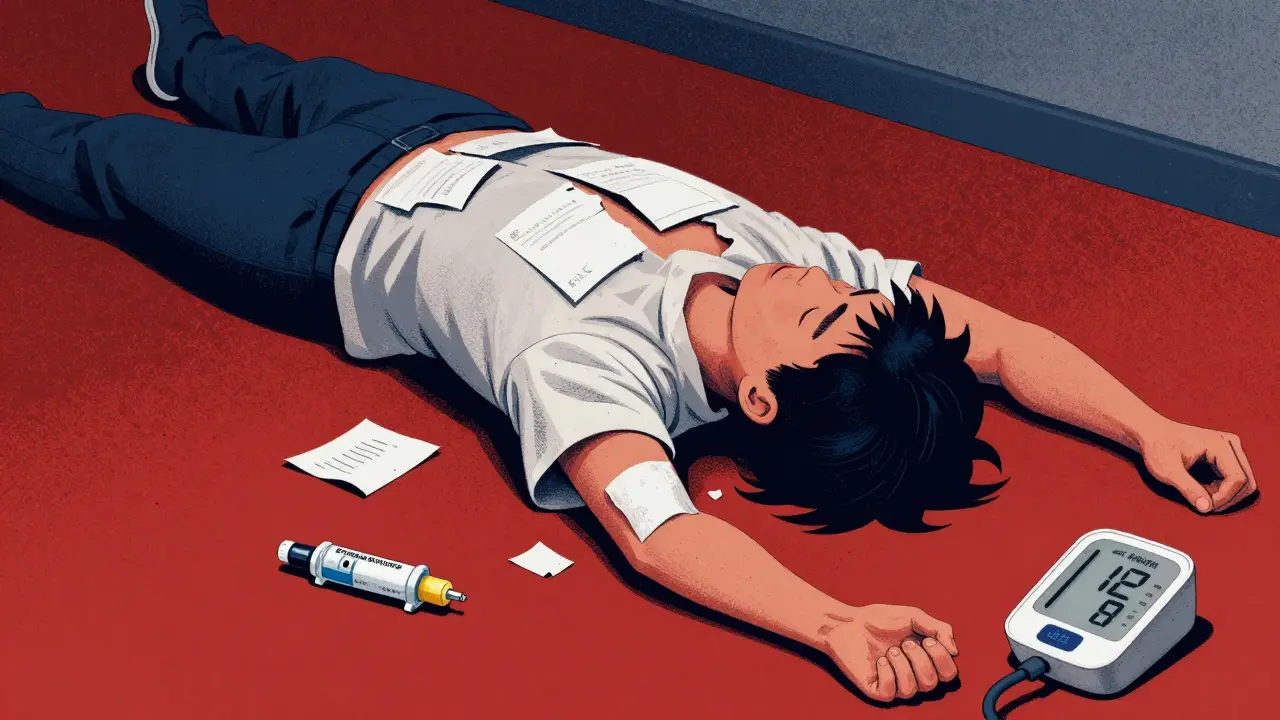
Severe reactions aren’t just bad - they’re deadly. And they happen faster than most people expect.
Anaphylaxis is the most dangerous. It’s not just a rash. It’s your body shutting down. Your blood pressure drops below 90 mmHg. Your airway swells. Your lungs tighten. Oxygen levels fall below 90%. You might feel a sense of doom, nausea, vomiting, or lose consciousness. This isn’t "feeling sick." This is a medical emergency.
Penicillin causes anaphylaxis in about 1-5 out of every 10,000 doses. But if you’ve had a mild reaction before? Your risk jumps. And if you’re HLA-B*15:02 positive? Taking carbamazepine increases your risk of severe skin reactions by 10 times.
Then there are Type IV reactions like Stevens-Johnson Syndrome (SJS) and Toxic Epidermal Necrolysis (TEN). These aren’t rashes. They’re burns. Your skin starts peeling off - sometimes 10% (SJS) or over 30% (TEN) of your body. Mortality rates? 5-15% for SJS. 25-35% for TEN. These patients need burn unit care. Fluids. Infection control. Intensive monitoring.
One Reddit user wrote: "I got a rash on day 3. Doctor said, ‘Keep taking it.’ By day 7, I had blisters. I spent 10 days in the ICU. My skin was falling off." That’s not an exaggeration. That’s a real case.
What’s the rule? If you have trouble breathing, low blood pressure, confusion, or more than 10% skin detachment - call 999. Epinephrine is the only thing that can stop anaphylaxis. Delay it, and you risk death.
Why Misdiagnosis Is the Silent Killer
Here’s the scary part: many severe reactions start as "mild rashes." And too often, they’re ignored.
A Drugs.com forum from April 2024 had 27 users who were told their rash was "just a side effect." They kept taking the drug. Three days later, they were in the ICU with skin detachment. One woman was prescribed a sulfa antibiotic for a UTI. Her doctor said, "It’s just a rash." She didn’t stop. By day 5, 25% of her skin had detached. She almost didn’t survive.
Why does this happen? Doctors in community clinics often don’t have the tools or time to assess severity properly. A 2023 AAAAI survey found only 45% of community practices use standardized severity tools. Academic hospitals? 85%. That gap kills.
And patients? They don’t know what to report. "I got a rash" isn’t enough. You need to say: "I got hives covering 15% of my chest and arms, started at 2 hours after the pill, and my face swelled up." Precision saves lives.
What You Should Do - Right Now
You don’t need to be a doctor to protect yourself. Here’s what to do:
- Track every reaction. Write down the drug name, dose, time you took it, and exactly what happened. Include photos if you can.
- Don’t guess. If you think you’re allergic, get tested. Skin tests for penicillin are 95% accurate. Blood tests for IgE exist. For delayed reactions, lymphocyte testing is available.
- Carry an epinephrine auto-injector if you’ve had a severe reaction. Even if it was years ago. Your risk doesn’t go away.
- Wear a medical alert bracelet. It tells emergency responders what you’re allergic to before they even ask.
- Ask for alternatives. If you’re allergic to penicillin, there are 10+ safe antibiotics. Don’t settle for "the first one they have."
The American College of Allergy, Asthma & Immunology has a free online severity calculator. It asks 12 questions - rash size, timing, breathing issues, swelling - and gives you a score. Under 20? Mild. 21-50? Moderate. Over 50? Emergency. Use it. It’s not magic. But it’s better than guessing.
The Future: Personalized Prevention
Things are changing. In 2025, the FDA will require all electronic health records to include severity assessment tools. By 2026, every new drug application in Europe must include a risk plan for severe reactions.
And the biggest shift? Genetic testing. Before prescribing carbamazepine to someone of Southeast Asian descent, doctors are now checking for HLA-B*15:02. If it’s positive? They avoid the drug. This single step cuts severe skin reactions by 70-80%.
That’s the future: not just treating reactions, but stopping them before they start.
Final Thought: Your Body Is Warning You
Medications save lives. But they can also hurt you - if you don’t listen.
A mild rash isn’t "just a rash." A swollen lip isn’t "no big deal." And if you feel like you’re going to pass out? That’s not anxiety. That’s your body screaming for help.
Know the signs. Speak up. Act fast. And don’t let anyone tell you it’s "probably nothing."

