Rickets Risk Assessment Tool
This tool helps you assess your risk of hereditary rickets based on family history, ethnicity, and lifestyle factors. Results are for informational purposes only and should not replace professional medical advice.
Enter your information above to see your risk assessment.
Rickets isn’t just a disease caused by a lack of sunshine or milk; it can run in families. Understanding how genetics rickets intersect helps doctors spot at‑risk children early and tailor treatment. Below you’ll get the facts you need to know whether your genes could be putting you or your kids at higher risk.
Quick Takeaways
- Rickets is a bone‑softening disorder driven primarily by low vitamin D, calcium, or phosphate.
- Specific gene mutations affect vitamin D metabolism, phosphate handling, or bone formation.
- Inheritance patterns include autosomal recessive, autosomal dominant, and X‑linked traits.
- Family history, ethnicity, and certain consanguineous marriages raise the odds of hereditary rickets.
- Genetic testing, combined with blood work, can confirm a hereditary form and guide therapy.
What Is Rickets?
Rickets is a pediatric disorder characterized by defective bone mineralization, leading to soft, deformed bones and growth plate abnormalities. The condition typically manifests as bowed legs, thickened wrists, and delayed motor milestones, and it reflects inadequate calcium or phosphate deposition in the growing skeleton. While nutritional deficiencies are the most common causes, the disease can also stem from inherited defects that disrupt the pathways governing vitamin D activation, phosphate regulation, or collagen formation.
The Vitamin D-Calcium Connection
Vitamin D is essential because it enables intestinal absorption of calcium and phosphate. When sunlight‑driven synthesis in the skin or dietary intake is insufficient, serum calcium drops, prompting the parathyroid glands to release parathyroid hormone (PTH). PTH tries to restore calcium by pulling it from bones, increasing renal reabsorption, and stimulating the conversion of inactive vitamin D (25‑hydroxyvitamin D) to its active form (1,25‑dihydroxyvitamin D) via the enzyme 1‑α‑hydroxylase.
In hereditary forms, the problem lies not in sunlight or diet but in the genes that control these biochemical steps. Mutations can block enzymes, alter hormone receptors, or impair phosphate transport, leaving the bone‑building process crippled even when nutrition looks adequate.
Genetics: The Underlying Blueprint
Genetics is the study of how DNA variations influence traits and disease risk. When a mutation disrupts a gene involved in vitamin D metabolism or phosphate balance, the resulting protein may be non‑functional, partially active, or overactive, each scenario potentially leading to rickets. Inherited rickets follows classic Mendelian patterns, meaning you can often predict risk based on family trees.
Key Genes Linked to Hereditary Rickets
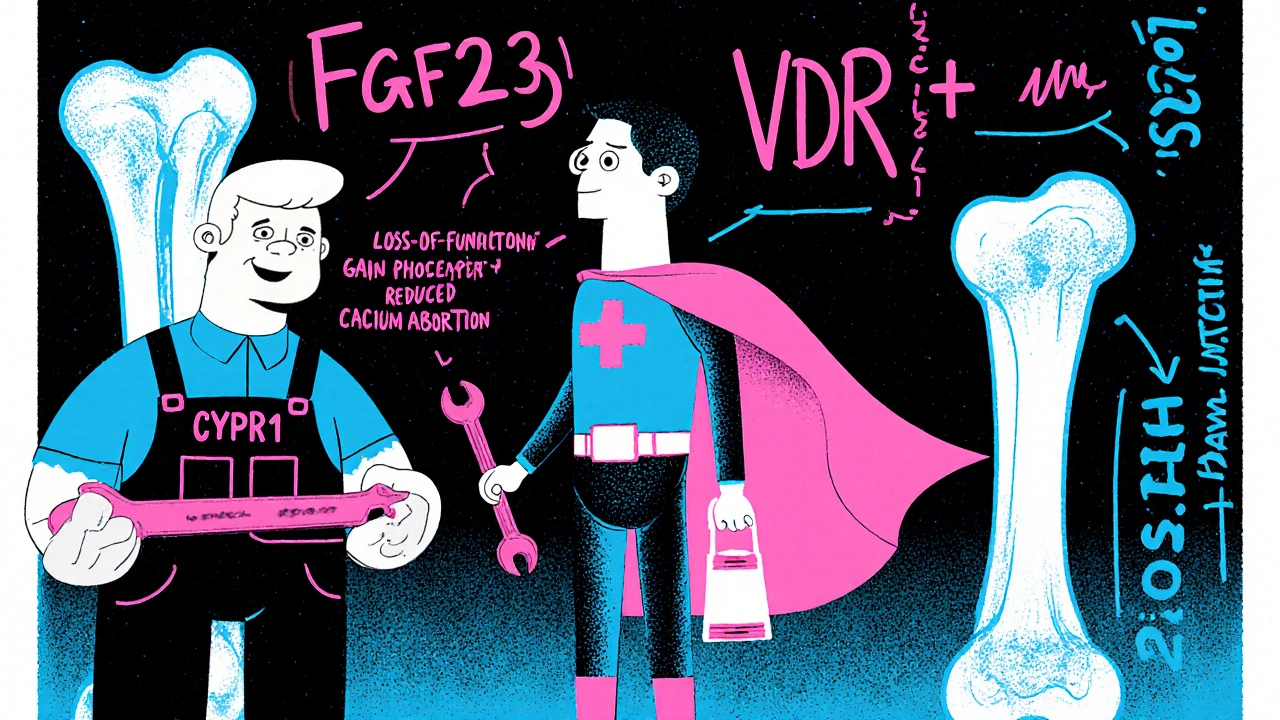
Scientists have identified a handful of genes where mutations reliably cause rickets‑like bone disease. Below is a snapshot of the most frequently encountered ones, the type of mutation, inheritance, and the biochemical impact.
| Gene | Mutation Type | Inheritance | Effect on Metabolism |
|---|---|---|---|
| CYP2R1 | Loss‑of‑function | Autosomal recessive | Impaired conversion of vitamin D to 25‑hydroxyvitamin D |
| VDR | Loss‑of‑function | Autosomal recessive | Defective vitamin D receptor; reduced calcium absorption |
| FGF23 | Gain‑of‑function | Autosomal dominant | Excess phosphate wasting; low serum phosphate |
| ALPL (TNSALP) | Loss‑of‑function | Autosomal recessive | Deficient tissue‑non‑specific alkaline phosphatase; poor bone mineralization |
| PHEX | Loss‑of‑function | X‑linked recessive | Elevated FGF23, leading to hypophosphatemia |
| DHCR7 | Loss‑of‑function | Autosomal recessive | Reduced cholesterol conversion to 7‑dehydrocholesterol, limiting skin‑derived vitamin D |
| NADSYN1 | Loss‑of‑function | Autosomal recessive | Impaired NAD synthesis, affecting vitamin D‑dependent enzymes |
Who Is More Prone? Risk Factors Beyond the Genes
Even with a pathogenic mutation, not everyone develops severe rickets. Several modifiers shape the final picture:
- Family history: A sibling or parent with confirmed genetic rickets raises your odds dramatically.
- Ethnicity: Certain populations-such as those of Middle Eastern, South Asian, or African descent-show higher frequencies of specific alleles like CYP2R1 or VDR variants.
- Consanguinity: Marriages between close relatives increase the chance of inheriting two copies of a recessive mutation.
- Sun exposure: Even a genetic defect can be mitigated by adequate UVB‑driven synthesis, whereas indoor living compounds risk.
- Dietary habits: Low dairy or fortified food intake worsens any underlying metabolic block.
Diagnosing Genetic Rickets
When a child presents with classic rickets signs, physicians start with routine labs: serum calcium, phosphate, alkaline phosphatase, PTH, and 25‑hydroxyvitamin D. If these results suggest a metabolic disturbance that doesn’t resolve with standard vitamin D supplementation, a genetic workup is warranted.
Typical diagnostic steps include:
- Detailed family pedigree to spot inheritance patterns.
- Targeted gene panel or whole‑exome sequencing focusing on known rickets‑related genes.
- Functional assays, such as measuring 1‑α‑hydroxylase activity in cultured fibroblasts for CYP2R1 mutations.
- Radiographic evaluation of growth plates (X‑ray of wrists/knees) to assess the severity of bone demineralization.
Genetic confirmation not only explains the cause but also guides treatment-some mutations respond better to phosphate supplements, others need high‑dose calcitrol.
Managing Hereditary Rickets
Therapy hinges on the specific metabolic defect:
- Vitamin D synthesis defects (CYP2R1, DHCR7): High‑dose oral calcifediol or active calcitriol bypasses the blocked step.
- Phosphate‑wasting disorders (FGF23, PHEX): Oral phosphate salts combined with low‑dose calcitriol stabilize serum phosphate.
- Alkaline phosphatase deficiency (ALPL): Enzyme‑replacement is experimental; current practice emphasizes aggressive calcium and phosphate supplementation.
- VDR mutations: Very high‑dose calcitriol may overcome receptor insensitivity, but monitoring for hypercalcemia is critical.
Regular monitoring-every 3‑6 months for serum calcium, phosphate, and urinary excretion-helps fine‑tune doses and avoids complications like nephrocalcinosis.
Lifestyle Tips to Reduce Risk
Even with a genetic predisposition, everyday habits can keep bones strong:
- Aim for 15‑30 minutes of midday sun exposure on uncovered arms and face, 2‑3 times a week, depending on skin tone.
- Include fortified dairy, fatty fish, or vitamin D‑supplemented plant milks in the diet.
- Ensure adequate calcium intake (1,000 mg/day for children 1‑8 years, 1,300 mg/day for teens).
- Encourage weight‑bearing activities-running, jumping, or dancing-to stimulate bone remodeling.
- Schedule routine pediatric check‑ups. Early detection of growth‑plate changes prevents severe deformities.
Future Directions: Gene Therapy and Precision Medicine
Researchers are exploring CRISPR‑based correction of CYP2R1 and VDR mutations in animal models. While still early, these approaches could eventually replace lifelong supplementation. Meanwhile, precision‑medicine platforms are integrating genetic data with biochemical profiles to predict optimal dosing for each mutation type.
Key Takeaway
If rickets runs in your family, don’t assume it’s just “lack of sunshine.” Genetic testing can uncover hidden defects, allowing doctors to prescribe the right form and amount of vitamin D, phosphate, or calcium-essential for keeping those little bones sturdy.

Can genetics cause rickets even with enough sunlight?
Yes. Mutations in genes such as CYP2R1 or VDR block the body’s ability to process or respond to vitamin D, so even abundant UVB exposure may not raise active vitamin D levels enough to mineralize bone.
What inheritance patterns are seen in hereditary rickets?
Both autosomal recessive (e.g., CYP2R1, VDR, ALPL) and autosomal dominant (e.g., FGF23) patterns occur, plus an X‑linked recessive form (PHEX) that predominantly affects males.
Should every child with rickets get genetic testing?
Testing is recommended when standard vitamin D therapy fails, when there’s a strong family history, or when biochemical labs show unusual patterns (e.g., low phosphate with normal vitamin D). A targeted gene panel can pinpoint the mutation quickly.
How is treatment different for phosphate‑wasting rickets?
Patients receive oral phosphate salts multiple times a day together with low‑dose active vitamin D (calcitriol). This combo restores serum phosphate while preventing secondary hyperparathyroidism.
Can adults develop genetic rickets?
Adults may present with osteomalacia, the adult counterpart of rickets, especially if they carry milder mutations that only become evident later in life when dietary vitamin D drops.


Joe Waldron
Vitamin D metabolism hinges on enzymes like CYP2R1; when that gene is knocked out, 25‑hydroxyvitamin D levels drop dramatically, leaving calcium absorption impaired. The body then ramps up PTH, which pulls calcium from bone-exactly what we see in rickets‑type lesions. Screening for these mutations early can spare kids from painful deformities; a simple blood panel plus targeted gene test does the trick. Parents should ask their pediatrician about a genetic work‑up if standard supplements don’t correct the labs.