Every year, nearly half a million people in the U.S. get Lyme disease - but only about 30,000 are officially reported. Why the gap? Because many cases are missed, misdiagnosed, or never seen by a doctor at all. Lyme disease isn’t just a summer nuisance. It’s a complex bacterial infection that can slip under the radar, then quietly spread through your body if not caught early. The good news? If you know what to look for and act fast, most people recover completely. The bad news? Delayed treatment can lead to months - or years - of pain, fatigue, and confusion.
How Lyme Disease Starts: The Tick That Changes Everything
Lyme disease isn’t spread by just any tick. It’s carried by two specific types: the blacklegged tick (Ixodes scapularis) in the Northeast and Midwest, and the western blacklegged tick (Ixodes pacificus) along the Pacific coast. These ticks are tiny - especially the nymphs, which are about the size of a poppy seed. That’s why so many people never notice they’ve been bitten. The bacteria that cause Lyme disease, Borrelia burgdorferi, live in the tick’s gut. But they don’t jump into your blood right away. It takes time. Most experts agree the tick needs to be attached for at least 24 to 36 hours before transmission happens. Some research suggests it can start as early as 15 hours, depending on the tick’s stage and the strain of bacteria. That’s why checking for ticks after being outdoors - especially in wooded or grassy areas - is so critical. Showering within two hours and doing a full-body check can cut your risk by up to 95%. Nymph ticks are the real problem. They’re small, quiet, and most active in spring and early summer - right when people are outside more. Adult ticks are easier to spot, but they’re less likely to transmit Lyme because they’re bigger and you’re more likely to notice and remove them quickly.The Three Stages of Lyme Disease - And What Happens in Each
Lyme disease doesn’t hit all at once. It unfolds in stages, each with its own signs and risks. Stage 1: Early Localized (1 to 28 days after the bite) This is when the infection is still near the bite site. About 70 to 80% of people develop a distinctive rash called erythema migrans - the classic “bull’s-eye” rash. It starts as a small red spot and expands over days, sometimes clearing in the center to form a ring. Not everyone gets it, though. Some people just feel off - fever, chills, fatigue, headache, muscle aches. These symptoms are easy to mistake for the flu. If you’ve been in tick country and feel sick after a hike or gardening, don’t brush it off. Stage 2: Early Disseminated (weeks to months after the bite) If the infection isn’t treated, the bacteria spread. Now you’re not just dealing with a rash. You might get multiple rashes in different places. Nerve problems can show up: facial palsy (drooping on one side of the face), numbness, or shooting pains. Heart issues like Lyme carditis can occur in 4 to 10% of untreated cases - causing dizziness, shortness of breath, or irregular heartbeat. This stage is serious but still treatable. Stage 3: Late Disseminated (months to years after the bite) This is what happens when Lyme is ignored for too long. Joint pain and swelling - especially in the knees - become common. Up to 60% of untreated patients develop arthritis. Neurological symptoms can include memory loss, trouble concentrating, and nerve pain. Some people describe it as “brain fog” that won’t go away. These symptoms can come and go, making it hard to connect them to a tick bite that happened a year ago.Treatment: What Works, When, and Why
The key to beating Lyme disease is speed. Antibiotics are highly effective - if you start them early. For early localized Lyme, doctors prescribe 10 to 21 days of oral antibiotics. Doxycycline is the go-to for adults and kids over 8. For younger children, pregnant women, or those allergic to doxycycline, amoxicillin or cefuroxime are used. Most people feel better within days. The rash fades, energy returns, and symptoms disappear. If the infection has spread - say, to the nerves or heart - treatment gets stronger. Intravenous antibiotics like ceftriaxone are given for 14 to 28 days. This isn’t a hospital stay for most people; many get IV meds at home through a portable pump. There’s one special case: prophylaxis. If you find an engorged blacklegged tick attached for more than 36 hours in a high-risk area (like Connecticut, Pennsylvania, or Wisconsin), a single 200mg dose of doxycycline taken within 72 hours of removal can prevent infection. This isn’t for everyone - only in specific situations. Talk to your doctor if you’re unsure.
Why Diagnosis Is So Hard - And Why It Matters
Here’s the frustrating part: blood tests for Lyme aren’t perfect - especially early on. In the first few weeks, your body hasn’t made enough antibodies for the test to catch. That means a negative test doesn’t rule out Lyme. In fact, early-stage tests miss up to 35% of true infections. That’s why doctors are taught to rely on symptoms first. If you have the bull’s-eye rash? No test needed. That’s the gold standard. Dr. Allen Steere, who first identified Lyme disease, said it yourself: the rash is pathognomonic - meaning it’s unmistakable. No lab test can prove it better than your eyes. But when the rash is absent - and many people don’t get it - testing becomes necessary. The standard two-tier test (ELISA followed by Western blot) works better later, when the infection has spread. But even then, false negatives happen. That’s why so many patients see three or more doctors before getting a correct diagnosis. One patient on Reddit waited 18 months and visited seven doctors before being told it was Lyme disease. In March 2023, the FDA approved the first new Lyme test in 20 years: the MiQLick test. It detects bacterial DNA in urine and shows 92% sensitivity in early disease. It’s not everywhere yet, but it’s a step forward.What Happens After Treatment? The Long Tail of Lyme
Most people recover fully. CDC data shows 87% of those treated within 30 days of symptoms are symptom-free within three months. But about 10 to 20% of patients - even after proper antibiotic treatment - continue to feel tired, achy, or mentally foggy for six months or longer. This is called Post-Treatment Lyme Disease Syndrome (PTLDS). It’s not an ongoing infection. Studies have found no live bacteria in these patients after treatment. The body’s immune system may still be reacting, or tissue damage from the infection could be lingering. PTLDS isn’t “chronic Lyme.” That term is used by some groups to describe persistent symptoms as evidence of ongoing infection - but major medical organizations like the Infectious Diseases Society of America (IDSA) say there’s no proof. Long-term antibiotics for PTLDS haven’t worked in clinical trials and can cause serious side effects like C. diff infections or antibiotic resistance. That doesn’t mean the suffering isn’t real. Dr. John Aucott at Johns Hopkins has studied PTLDS for years. His patients describe debilitating fatigue, joint pain, and brain fog that disrupts work, relationships, and daily life. Treatment focuses on symptom management: physical therapy, pacing activities, sleep support, and sometimes low-dose anti-inflammatories.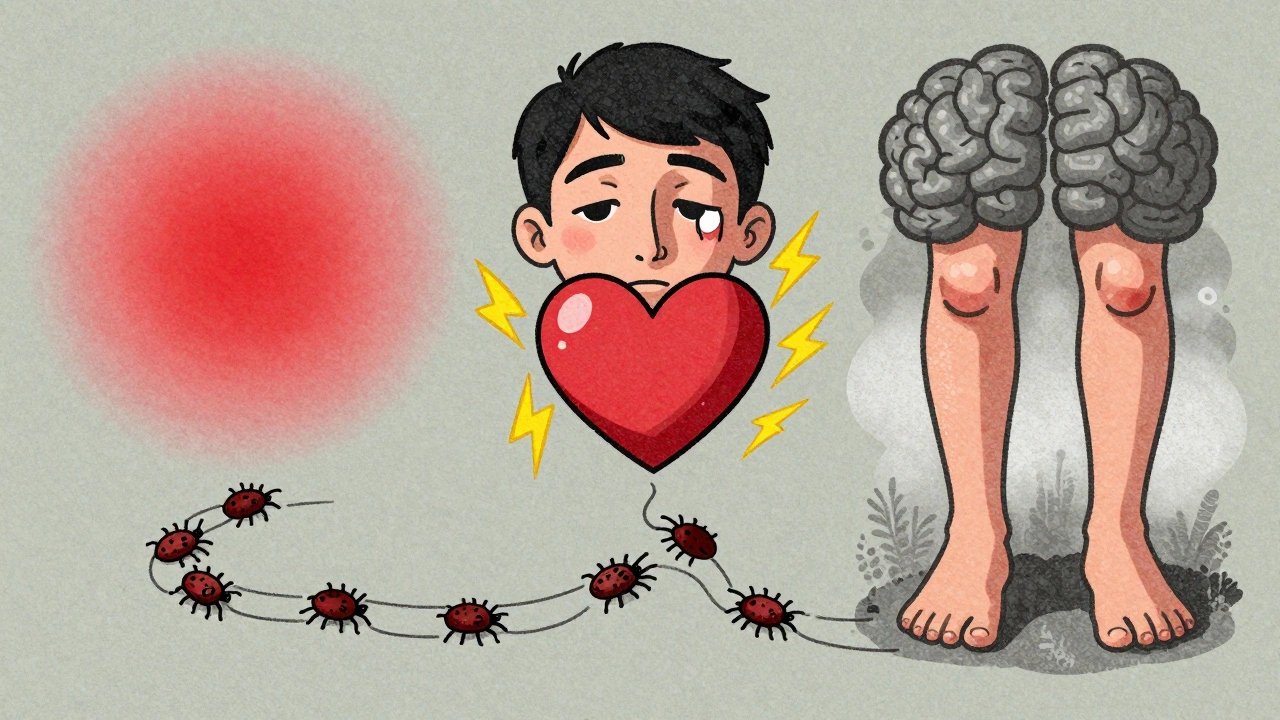
What’s Changing in Lyme Disease Care?
The landscape is shifting. Climate change is pushing ticks farther north. A 2021 study showed Ixodes scapularis habitats expanded 50% in Canada over 20 years. Lyme is no longer just a Northeast problem - it’s showing up in states like Minnesota and even parts of the Pacific Northwest. A new vaccine, VLA15, developed by Valneva with Pfizer, showed 70 to 96% effectiveness in phase 2 trials. It’s now in phase 3 testing and could be available by 2027. Meanwhile, researchers at NIAID are working on an mRNA vaccine - similar to the ones used for COVID - expected to enter human trials in mid-2024. Economic costs are rising too. Lyme disease now costs the U.S. over $2.6 billion a year in medical bills and lost productivity. That’s more than $5,500 per case on average.What You Can Do Right Now
- Check for ticks daily after being outside. Pay attention to armpits, groin, scalp, and behind the knees. - Shower within two hours of coming indoors - it helps wash off unattached ticks. - Remove ticks with tweezers - grab close to the skin and pull straight up. Don’t twist or squeeze. - Save the tick in a sealed bag if you can. It helps doctors assess risk. - Don’t wait for a rash if you feel sick after a tick bite. See a doctor immediately. - Know your risk zone. If you live in or visit Connecticut, Massachusetts, New York, Pennsylvania, Wisconsin, or other high-incidence states, be extra vigilant.When to Call Your Doctor
Call right away if: - You have a red, expanding rash - especially with a clear center - You develop fever, chills, fatigue, or muscle aches after a tick bite - You notice facial drooping, dizziness, or heart palpitations - You have joint swelling that comes and goes Don’t wait for a test. Don’t hope it’ll go away. Early treatment changes everything.Can you get Lyme disease more than once?
Yes. Getting Lyme disease once doesn’t give you immunity. You can be bitten again and infected again. That’s why ongoing prevention - tick checks, repellents, protective clothing - is essential even if you’ve had it before.
Do all ticks carry Lyme disease?
No. Only blacklegged ticks (Ixodes species) carry the bacteria that cause Lyme disease in the U.S. Other ticks, like dog ticks or lone star ticks, can carry different illnesses - like Rocky Mountain spotted fever or STARI - but not Lyme.
Is Lyme disease contagious between people?
No. You can’t catch Lyme disease from another person through touch, kissing, sex, or blood transfusion. The only way it spreads is through the bite of an infected tick. There’s no evidence it passes from mother to baby during pregnancy if treated properly.
Can pets get Lyme disease and pass it to me?
Dogs and cats can get Lyme disease, but they can’t directly infect humans. However, ticks that bite your pet can crawl off and bite you. That’s why using tick preventatives on pets and checking them after walks is part of protecting yourself.
Are natural remedies like essential oils or herbs effective for Lyme?
There’s no scientific proof that essential oils, herbal supplements, or alternative therapies cure Lyme disease. While some may help with symptom relief - like turmeric for inflammation - they don’t kill the bacteria. Relying on them instead of antibiotics can allow the infection to spread and cause serious, long-term damage.
What should I do if I find a tick on me?
Use fine-tipped tweezers to grasp the tick as close to the skin as possible. Pull upward with steady, even pressure. Don’t twist or crush it. Clean the area with soap and water. Save the tick in a sealed container with a damp cotton ball, and note the date. Contact your doctor - especially if the tick was engorged or attached for more than 24 hours.
Can Lyme disease be cured?
Yes - when caught early. Most people treated with the right antibiotics in the first few weeks recover completely. The longer it goes untreated, the harder it becomes to reverse damage. But even in late stages, treatment can stop progression and improve symptoms. The goal is to prevent it from ever getting that far.


Ollie Newland
Just had a tick removed last week after a hike in Vermont. Didn’t see a rash, but I’ve been dizzy and fatigued since. Went to my doc and they were like ‘probably nothing’ - but I pushed for doxycycline prophylaxis since it was engorged and attached over 48hrs. Got the 200mg dose within 72. Fingers crossed. That FDA-approved MiQLick test sounds like a game-changer if it rolls out widely.