I was gobsmacked the first time I saw a patient’s ankles deflate after the right med tweak. If you’ve watched loop diuretics flop on stubborn swelling, you know it feels like pushing a boulder uphill. Even those famous ‘water pills’—Lasix, bumetanide, torsemide—run into brick walls, especially in heart failure or kidney issues. But here’s the kicker: when loops hit that ceiling, switching gears to a thiazide like HCTZ or metolazone can sometimes work wonders even when Lasix is yelling ‘uncle.’ The trick is knowing when and why.
Why Loop Diuretics Sometimes Hit a Wall
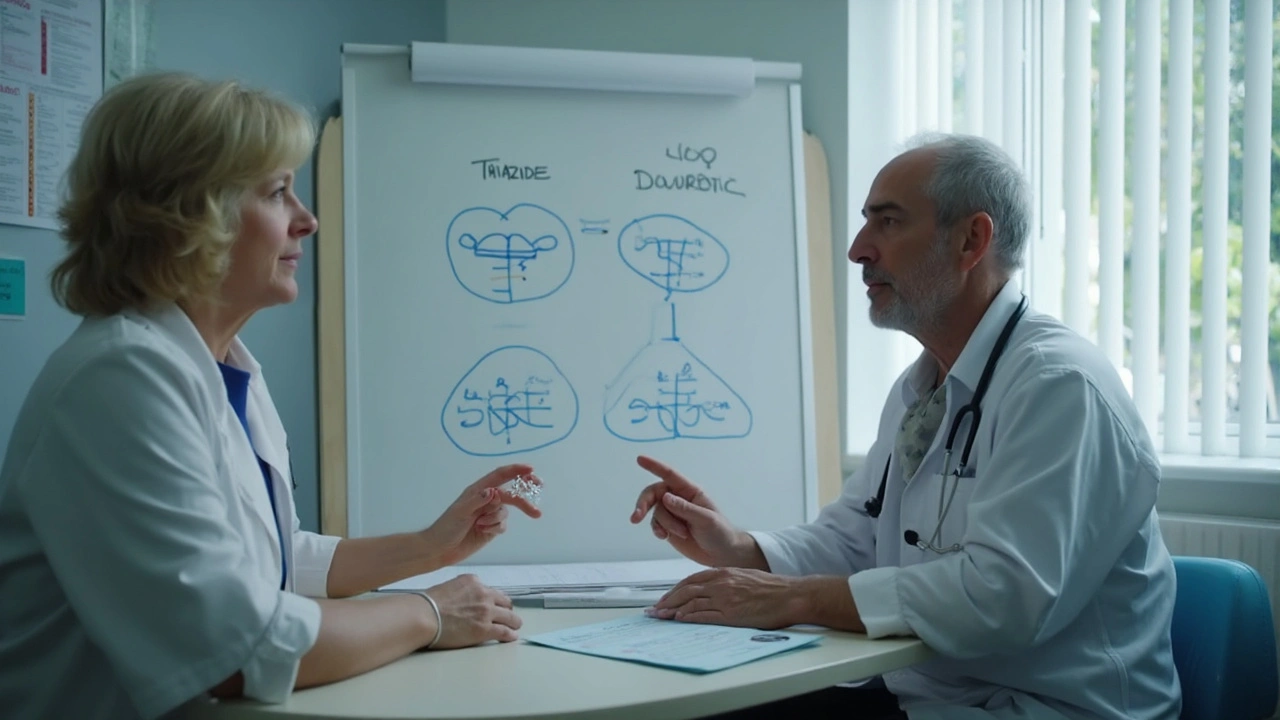
Let’s start with why Lasix, the classic go-to loop diuretic, isn’t always a slam dunk. Loops act on a part of your kidney called the ascending limb of the loop of Henle—think of it as opening the dam wide for sodium and water to pour out. For most, they’re potent and fast. But after a while, your body adapts. The kidneys start reabsorbing salty water elsewhere, especially in the distal tubule. The more Lasix you push, the more your body figures out other sneaky ways to reabsorb fluid, like a leaky faucet that just won’t quit.
What’s wild is some people, especially those with long-term kidney or heart disease, just stop responding to typical doses. That’s called diuretic resistance. You could double or triple the Lasix and barely budge that stubborn edema. There’s actually a name for it—the ‘braking phenomenon.’ Your body literally slams the brakes and throws out all the tricks in the book to keep the salt in.
Plus, oral Lasix gets annoying when the gut is waterlogged with fluid—absorption tanks and you wind up peeing out barely any extra fluid. This happens a lot in hospital wards, but I’ve seen it plenty in clinics here in London too. Chronic kidney disease patients or those with severe heart failure are most at risk. If you check the textbooks, up to 30% of congestive heart failure patients will hit some level of diuretic resistance during their treatment.
So, when you’re staring at ballooning ankles, tight shoes, and unbudging scale numbers, it’s time for a rethink.
How Thiazide Diuretics Can Break the Plateau
Now for the cool bit—what if you could trick the kidneys? Enter the thiazide family: hydrochlorothiazide (HCTZ), metolazone, and others. They go after the distal convoluted tubule—the next station after the loop of Henle. By knocking out sodium reabsorption there, these meds block the kidney’s backup plan to hold onto salt and water. This is why thiazides work so well in combo with loops—they attack from a different angle.
Doctors sometimes call this the ‘sequential nephron blockade.’ Sound posh, but all it means is you’re closing both doors instead of one, so the body has far fewer places to sneak salt back in. Metolazone is the real star when edema gets nasty. Unlike HCTZ, metolazone keeps on working even when your kidneys are slowing down—no wonder it’s a hospital favorite for rough cases. I’ve seen people lose liters, yes, liters, of excess fluid in 24 hours after starting metolazone plus a loop diuretic. It’s almost as if you flipped a switch on the body’s stubbornness.
When does this double-attack make sense? It’s especially useful if you’ve maxed out your loop diuretic—say, Lasix 80mg twice daily—and there’s still loads of swelling. This happens a lot in advanced heart failure, severe liver disease, and chronic kidney disease. Ever try to strap shoes on a nephrotic syndrome patient? That’s when the thiazide plus loop trick comes to the rescue.
If you’re looking for other options when Lasix disappoints, it’s worth skimming this resource on alternatives to Lasix. It cuts through the choices and explains what might work for tough edema.
Real Scenarios: When HCTZ or Metolazone Beats the Loop
Case studies make this come alive. One of my regulars, Mrs. Golding, came in last summer swollen from ankles right up the calves—Lasix at 120mg daily was barely touching it. Her kidney numbers were creeping, so I held off on spironolactone. Switched to a modest metolazone dose with her morning Lasix and she was down three kilos in a week. Shoes finally fit. The trick? We timed both pills together: thiazide just 30 minutes before the loop. It’s a game-changer for absorption.
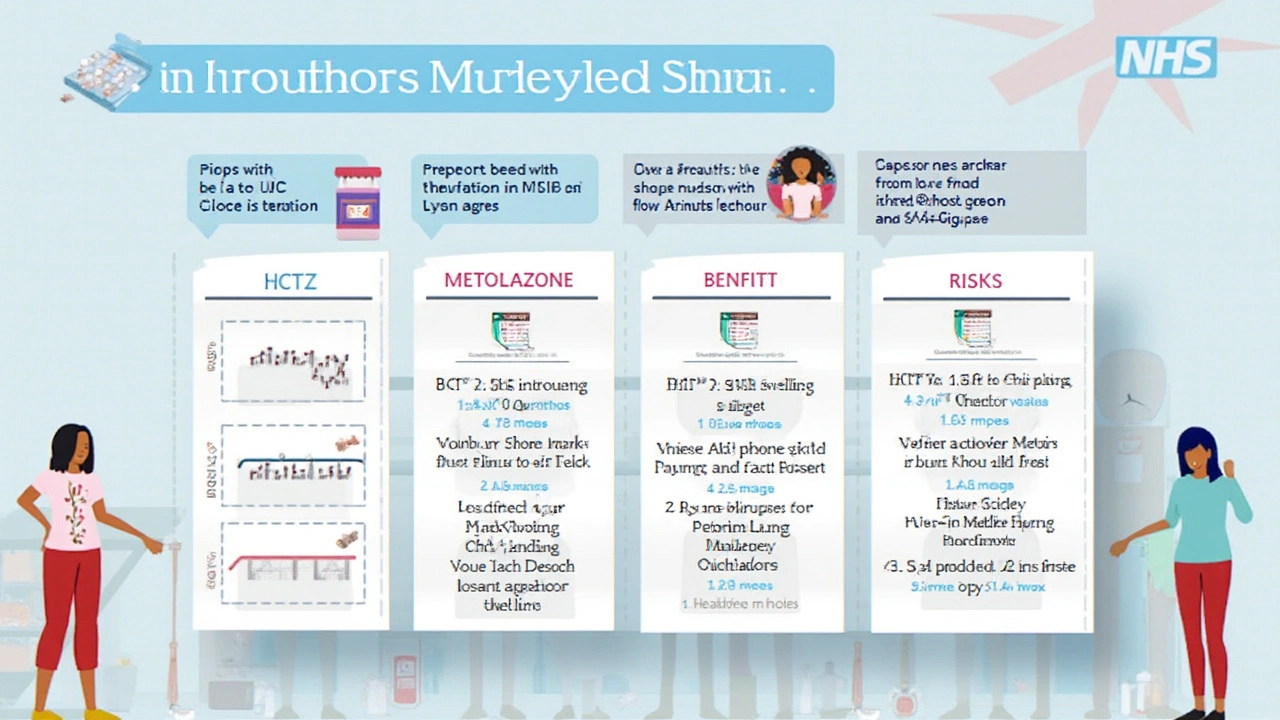
Thiazides also shine in the elderly, where loop diuretics often mean fainting spells or wild swings in potassium. With HCTZ, you can tightly control the water loss and nudge the pressure down gently—great for folks with high blood pressure who run out of options. But metolazone trumps HCTZ if the kidneys aren’t playing ball. That ‘thiazide-like’ structure means it still works when the glomerular filtration rate (GFR) drops under 30 ml/min. For context, HCTZ throws in the towel at that point—almost useless for people on the edge of dialysis.
If you want the raw numbers on this, check out this data:
| Diuretic | Works when GFR <30 ml/min? | Effective combo with loop? |
|---|---|---|
| HCTZ | No | Sometimes |
| Metolazone | Yes | Yes |
| Indapamide | Yes (but weaker than metolazone) | Rarely used in combo |
Heart failure clinics in London majorly favor metolazone for ‘crash’ fluid removal, especially if the loop diuretic starts yawning at your maximum dose. Even respiratory teams will use this combo for refractory pulmonary edema, sometimes just for a few days to get patients back on their feet.
What to Watch: Side Effects, Pitfalls, and Practical Tips
None of these tricks are risk-free. If you’re stacking loop and thiazide diuretics, you’d better be ready to monitor bloodwork—sodium and potassium drop fast, and dehydration can sneak up. I had a chap, early 60s, land in A&E after a double whammy with both diuretics blitzed his sodium into the danger zone. Especially for anyone older or on blood pressure meds, start slow and watch the labs every couple of days at first.
A neat tip: always remind people to take metolazone at least 30 minutes before their loop diuretic. The synergy is strongest that way. And since some doctors worry about ‘overdiuresing’—pulling off too much fluid—mark your initial goals carefully. Daily weights at home, regular kidney checks, and sipping fluids instead of gulping are key tricks.
Which side effects should make you pause? Dizziness, confusion, muscle cramps, or new palpitations can mean your salts are off. This goes double for those on ACE inhibitors or ARBs, where the risk of kidney strain is higher. Keep an eye out for gout flares—thiazides, particularly HCTZ, can spike uric acid. The upside? Most times, cautious use for a few days works wonders, and a quick med review or blood test can catch trouble early.
- Always check potassium and sodium 1–2 days after starting or changing thiazide in combination
- Instruct patients to record daily weights (ideally morning, after the loo, before breakfast)
- Metolazone often needs a lower starting dose compared to HCTZ—0.5 to 2.5 mg is plenty for most people
- If severe cramps or thirst hit, stop the thiazide and get checked—these can signal dangerous salt loss
- Warn about gout or joint pain with HCTZ, especially in those with a history
Clever Combinations and the Future of Diuretic Tweaking
Medicine never stands still. Doctors and researchers are constantly looking for new angles to treat diuretic resistance. Some are mixing metolazone with higher loop doses, others try adding acetazolamide or SGLT2 inhibitors—especially in tough heart failure. Digital health tools are picking up steam too—imagine a world where your phone pings your care team if your weight jumps two kilos overnight. It’s already happening at clinics in London and across the UK.
Tablets are getting smarter. Slow-release versions of thiazide-like diuretics may tighten up control, cut side effects, and make it easier for patients juggling lots of meds. I see more nurses and pharmacists getting involved in frequent check-ins by phone or app, catching problems before anyone lands in hospital. The takeaway? Diuretic resistance isn’t a dead end. With careful combos, and eyes peeled for side effects, most people do get back on track—even after Lasix runs dry.
At home, my son Oliver loves hearing how doctors ‘unlock secret codes’ in the body. That’s exactly what these diuretic combos do—they outsmart the system. So, if you find yourself or someone you love stuck in the swelling cycle, remember: you’re not alone, and there are real, proven tweaks worth trying—just make sure you loop in your medical team before making a move.

Asia Lindsay
Great breakdown! The way you highlighted the sequential nephron blockade really helps clinicians visualize the combo. 👍 Keep sharing these practical pearls; they're gold for bedside decision‑making. 💡 Remember to pair doses 30 minutes apart for optimal synergy. 💪 Your enthusiasm makes a big difference in patient outcomes.