When you're undergoing chemotherapy, the last thing you want is to feel worse after the treatment starts. But for about 5% of patients, something unexpected happens: their body reacts badly to the drugs meant to save their life. These are called chemotherapy hypersensitivity reactions. They can start with a tiny itch or a flush of warmth - and within minutes, turn into a life-threatening emergency. Knowing the signs and what to do can make all the difference.
What Exactly Is a Chemotherapy Hypersensitivity Reaction?
It’s not just nausea or fatigue. A chemotherapy hypersensitivity reaction is your immune system overreacting to the drug. It treats the chemotherapy as an invader, triggering a flood of chemicals like histamine and cytokines. This causes symptoms that look a lot like a severe allergy - even if you’ve never been allergic before. These reactions aren’t the same as infusion reactions, which are caused by the drug irritating your body directly. But they often feel the same. That’s why doctors and nurses have to treat every sudden symptom during chemo as potentially serious until proven otherwise. The most common culprits? Platinum drugs like carboplatin and oxaliplatin, taxanes like paclitaxel and docetaxel, and certain monoclonal antibodies like rituximab and trastuzumab. Even drugs you’ve taken safely before can suddenly trigger a reaction - especially after multiple cycles.Signs to Watch For - From Mild to Life-Threatening
Symptoms don’t always come all at once. They often start small and get worse fast. Pay attention to any new feeling during or right after your infusion.- Skin and eyes: Itchy skin, hives, flushing (sudden redness), or swelling around the eyes, lips, or tongue. Up to 72% of patients report itching, and 65% develop rashes.
- Respiratory: Feeling like you can’t catch your breath, wheezing, chest tightness, or coughing. About 45% of moderate reactions involve breathing trouble.
- Heart and circulation: Dizziness, fainting, rapid heartbeat (over 100 bpm), low blood pressure (below 90 systolic), or chest pain. These are red flags for anaphylaxis.
- Gut: Nausea, vomiting, stomach cramps, or diarrhea. These can be mistaken for chemo side effects - but if they show up suddenly during infusion, they’re likely part of a reaction.
- Neurological: A strange sense of doom, anxiety, tingling in the mouth, or even confusion. Nearly half of patients with anaphylaxis report feeling like something terrible is about to happen.
- General: Chills, fever, sweating, or a metallic taste in your mouth. These are common with platinum drugs and can be early warning signs.
When Do These Reactions Usually Happen?
Timing matters. Most reactions happen during the infusion or within the first hour after it ends. But some can show up 12 to 48 hours later - which is why you’re still monitored after you leave the chair. The risk changes with each cycle. For example:- With carboplatin, the first few cycles are usually safe. But after the sixth infusion, the chance of a reaction jumps to 6.5%. By the eighth cycle, it’s nearly 27%.
- Oxaliplatin causes reactions in about 19% of patients, but severe ones are rare - only 1.6%.
- Paclitaxel and docetaxel often trigger reactions during the first or second treatment.
How Doctors Diagnose It
There’s no single test. Diagnosis is based on what you feel, when it happens, and what drug you got. Doctors look for:- Sudden symptoms during or right after chemo
- Two or more body systems involved (like skin + breathing, or heart + stomach)
- No other explanation (like infection or asthma flare)
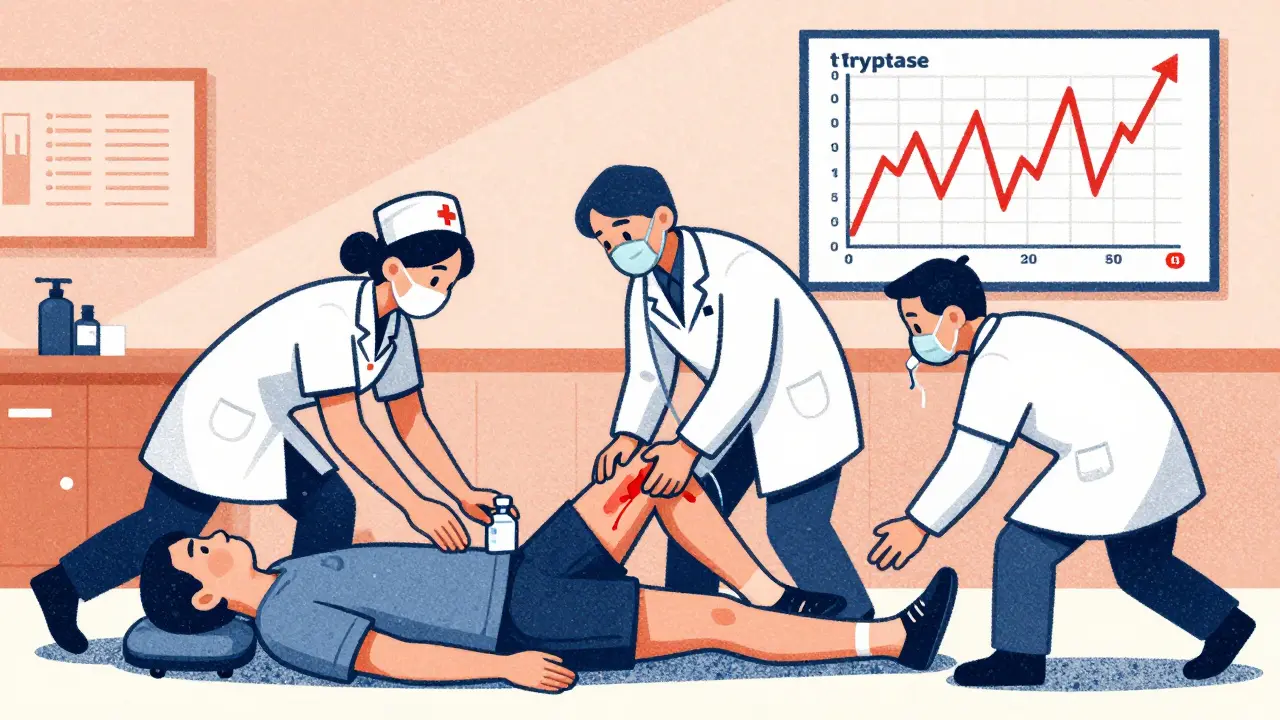
What to Do If a Reaction Happens
The response depends on how bad it is.Mild Reaction (Itching, mild rash, slight flushing)
- Stop the infusion
- Give diphenhydramine (Benadryl) 25-50 mg IV
- Give dexamethasone 10-20 mg IV
- Monitor vital signs for 30 minutes
- If symptoms clear, restart the infusion slowly
Moderate Reaction (Facial swelling, wheezing, more intense rash)
- Stop the infusion
- Give the same meds as above
- Start oxygen if breathing is affected
- Wait until symptoms fully resolve before considering restarting
- Slow down the infusion rate next time
Severe Reaction (Anaphylaxis - low blood pressure, trouble breathing, fainting)
- STOP THE INFUSION IMMEDIATELY
- Give epinephrine (adrenaline) 0.3-0.5 mg into the thigh muscle (1:1,000 solution)
- Call for emergency help
- Put you flat on your back with legs raised to improve blood flow
- Give oxygen and IV fluids
- Repeat epinephrine every 5-15 minutes if symptoms return
- Prepare for intubation if airway swells
How to Prevent Reactions Before They Start
For drugs known to cause reactions - like taxanes - hospitals use premedication:- Dexamethasone 20 mg IV, 12 and 6 hours before infusion
- Diphenhydramine 50 mg IV, 30 minutes before
- Famotidine 20 mg IV, 30 minutes before
What You Can Do - Patient Actions That Save Lives
You’re not just a patient. You’re part of the safety team.- Report every single symptom - even if you think it’s nothing. A metallic taste? A warm flush? Tell your nurse.
- Know your history. Did you have a reaction before? Tell your oncology team every time you start a new cycle.
- Ask: “Is this drug known to cause reactions?” If it is, ask if premeds are planned.
- Don’t ignore delayed symptoms. If you get hives or swelling hours after leaving the clinic, call your oncology unit. Don’t wait until tomorrow.
- Carry a list of your chemo drugs and past reactions. Keep it in your wallet or phone.

What Hospitals Must Have Ready
Every chemo unit should have an anaphylaxis kit within reach - no exceptions. That kit must include:- Epinephrine (1:1,000) auto-injectors or vials with syringes
- IV diphenhydramine and corticosteroids
- Oxygen delivery system
- IV fluids and tubing
- Airway management tools (mask, bag, intubation equipment)
What Happens After a Reaction?
If you had a mild reaction, you may be able to continue treatment with premeds and slower infusions. If you had a severe reaction, you’ll likely switch to a different chemo drug. Your team will test alternatives to find one that works without triggering your immune system. In rare cases, you may be referred to an allergy specialist for skin or blood testing. This isn’t routine - but it helps if you need to reuse a drug you’ve reacted to before.Final Thought: Don’t Wait for the Worst
Chemotherapy hypersensitivity reactions are rare - but they’re not random. They follow patterns. They have signs. And they’re treatable - if caught early. The difference between a scary moment and a fatal one often comes down to one thing: someone speaking up. If you feel something off during chemo - say something. If you’re a nurse or doctor - don’t dismiss a symptom because it’s “mild.” Don’t wait for the textbook case. Real emergencies start small. Your body is giving you clues. Listen.Can you have a chemo allergy without knowing it before?
Yes. Many patients have their first reaction after several cycles, even if they’ve taken the same drug safely before. The immune system can become sensitized over time. This is especially common with platinum drugs like carboplatin.
Is anaphylaxis from chemo common?
True anaphylaxis is rare - affecting less than 1% of patients overall. But it’s deadly if missed. About 0.5% of fatal reactions in chemo patients are due to untreated anaphylaxis. That’s why every reaction is treated as serious until proven otherwise.
Can I get re-infused after a reaction?
For mild reactions, yes - with premedication and a slower infusion. For severe reactions, you’ll usually switch drugs. But if no alternatives exist, doctors can try desensitization - a controlled process over several hours to gradually build tolerance under strict monitoring.
Do antihistamines stop anaphylaxis?
No. Antihistamines help with itching and hives, but they don’t reverse low blood pressure, airway swelling, or cardiac collapse. Epinephrine is the only medication that can stop anaphylaxis. Delaying it increases the risk of death.
What should I do if I feel symptoms at home after chemo?
Call your oncology team immediately. Don’t wait. Symptoms like swelling, trouble breathing, dizziness, or a rash that spreads after leaving the clinic could be a delayed reaction. If you’re having trouble breathing or feel faint, call emergency services. Don’t drive yourself.
Are there long-term risks after a chemo reaction?
If treated quickly, most patients recover fully without lasting damage. The main risk is being forced to stop an effective treatment. That’s why prevention and early response are so important. In rare cases, repeated reactions can lead to chronic sensitivities, but this is uncommon.

roger dalomba
Wow. Another 10-page essay on how to not die from chemo. Can we just get a pill that says ‘don’t be allergic’? 😴