What Is Aspirin-Exacerbated Respiratory Disease?
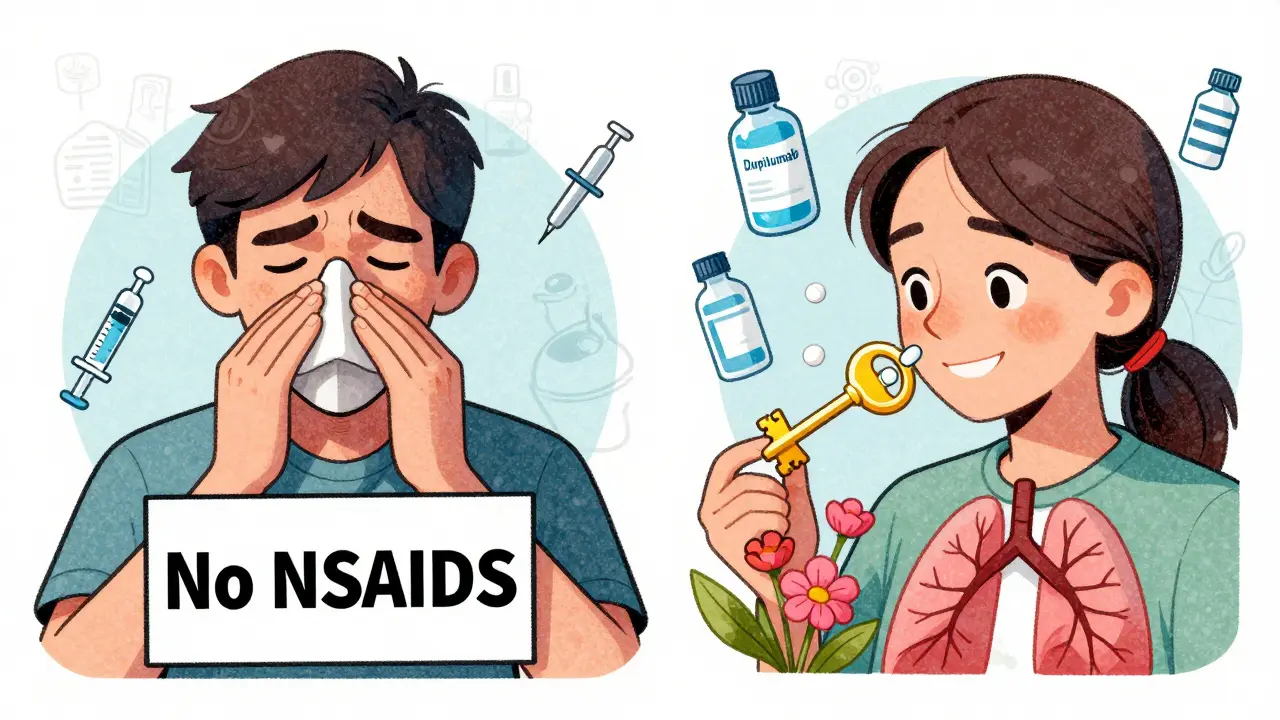
Aspirin-Exacerbated Respiratory Disease, or AERD, is not just a bad reaction to painkillers. It’s a chronic condition that affects the lungs and sinuses, often starting in adulthood. People with AERD have three things in common: asthma, nasal polyps, and severe breathing problems after taking aspirin or common NSAIDs like ibuprofen or naproxen. This combination is also called Samter’s Triad, named after the doctors who first mapped it out in the 1960s.
AERD doesn’t show up overnight. Most people notice symptoms between ages 20 and 50. Women are slightly more likely to develop it than men. About 7% of all adults with asthma have AERD-and if you have nasal polyps along with asthma, your chances jump to 14%. Unlike regular allergies, AERD isn’t triggered by pollen or pet dander. It’s caused by how your body handles inflammation chemicals, especially when you take aspirin or NSAIDs.
How Is AERD Diagnosed?
There’s no single blood test or scan that confirms AERD. Diagnosis relies on your medical history and what happens when you’re exposed to aspirin. If you’ve had asthma flare-ups after taking ibuprofen or aspirin, that’s a big red flag. So are recurring nasal polyps that keep coming back after surgery.
When the history isn’t clear, doctors use a supervised aspirin challenge. This isn’t something you do at home. You go to a clinic with emergency equipment on standby. Starting with a tiny dose-20 to 30 milligrams-you’re given increasing amounts every 90 to 120 minutes. If your airways tighten, your nose gets stuffy, or you start wheezing, the test stops. A reaction at or before 325 mg confirms AERD. This test is the gold standard, backed by guidelines from the American Academy of Allergy, Asthma & Immunology.
Other clues help support the diagnosis. Blood tests often show high eosinophils-over 500 cells per microliter-which means your body is in constant low-grade inflammatory mode. Urine tests can detect elevated leukotriene E4, a key inflammation driver in AERD. About 89% of patients have this marker when symptoms are active.
What Happens When You Take Aspirin or NSAIDs?
For someone with AERD, taking aspirin or NSAIDs doesn’t just cause a stomach upset. It triggers a full-blown respiratory reaction. Within 30 to 120 minutes, you might get: severe nasal congestion, loss of smell, wheezing, chest tightness, or even a full asthma attack. Some people vomit or break out in hives. These reactions aren’t allergic in the classic sense-they’re caused by a biochemical imbalance in your body’s inflammatory pathways.
When COX-1 enzymes are blocked by aspirin or NSAIDs, your body shifts production toward leukotrienes. These chemicals cause swelling in your sinuses and airways, attract eosinophils, and make mucus thicker. That’s why polyps grow back fast and asthma gets worse. Even if you avoid NSAIDs, the disease keeps progressing because your body is stuck in this overactive inflammation loop.
How Is AERD Managed Without Desensitization?
Many patients try to manage AERD by avoiding aspirin and NSAIDs. But that’s not enough. The disease keeps getting worse even without triggers. So treatment focuses on controlling inflammation.
First-line therapy starts with steroid sinus rinses. Using a neti pot with 50 to 100 mg of budesonide twice a day can shrink polyps by 30-40% in just eight weeks. Combined with daily fluticasone nasal sprays, this improves congestion scores by 35% on the SNOT-22 scale.
For asthma, medium-dose inhaled corticosteroids paired with long-acting bronchodilators-like fluticasone/salmeterol-are standard. These improve lung function by 15-20% in most patients. But if symptoms persist, doctors turn to leukotriene modifiers. Zileuton, which blocks leukotriene production, works well for about 28% of patients. Montelukast helps a bit, but only 15% report major improvement.
For the most severe cases, biologics like dupilumab or mepolizumab are game-changers. Dupilumab, given as a biweekly shot, reduces polyp size by 55% and improves quality of life scores by 40% in 16 weeks. Mepolizumab cuts eosinophil counts by 85% and reduces the need for repeat sinus surgeries by over half. These drugs don’t cure AERD, but they slow it down significantly.

What Is Aspirin Desensitization-and Why Does It Work?
Aspirin desensitization is the only treatment that changes the long-term course of AERD. It’s not a cure, but it stops the disease from progressing. The process starts with the same supervised challenge used for diagnosis-but instead of stopping at the reaction, you keep going. You’re given small, increasing doses until you can tolerate 325 mg without symptoms. Then, you start taking 650 mg daily, twice a day.
Once desensitized, your body adapts. The inflammation pathway resets. Studies show that after desensitization, patients need fewer oral steroid bursts-dropping from over four per year to just one. Nasal polyp recurrence after sinus surgery falls from 85% to 35% within two years. Smell function improves dramatically: patients go from barely recognizing scents to regaining the ability to smell coffee, flowers, or even their own food.
The procedure is safe when done right. At top centers like Brigham and Women’s Hospital, 98% of patients complete desensitization successfully. It’s done over two days, outpatient, with continuous monitoring. You might feel nasal stuffiness or mild wheezing during the process, but serious reactions are rare in controlled settings.
Who Should Get Aspirin Desensitization?
Not everyone with AERD is a candidate. The best candidates are those who:
- Have recurring nasal polyps requiring surgery
- Have poorly controlled asthma despite standard treatments
- Are willing to take daily aspirin long-term
Doctors strongly recommend desensitization after sinus surgery. Studies show that combining surgery with desensitization cuts polyp recurrence to just 25-30% at two years-compared to 60-70% with surgery alone.
But there are limits. Desensitization is not safe for people with:
- Severe heart disease or recent heart attack
- Active peptic ulcers or bleeding disorders
- History of aspirin-induced anaphylaxis without prior desensitization
- Inability to take aspirin daily without missing doses
About 15% of patients are ruled out due to these risks. Missing two or three doses in a row can undo the desensitization-you’ll need to start over.
What Are the Downsides and Challenges?
Aspirin desensitization works-but it’s not easy. About 22% of long-term users develop stomach issues like heartburn or ulcers. Taking aspirin with food helps, and some patients switch to enteric-coated aspirin. Still, GI side effects are the most common reason people stop.
Cost and access are huge barriers. There are only about 35 specialized AERD centers in the U.S., mostly in big cities. Rural patients often can’t reach one within 100 miles. Biologics like dupilumab cost over $30,000 a year-many patients can’t afford them without insurance. A 2023 survey found 65% of patients with incomes under $50,000 say cost blocks their treatment.
Even the aspirin challenge can be scary. About 32% of patients report high anxiety during the procedure. But most say the relief afterward makes it worth it.
What’s New in AERD Treatment?
The field is moving fast. A new drug called MN-001 (tipelukast), which blocks two inflammation pathways at once, showed a 60% drop in leukotriene levels in early trials. Combining dupilumab with aspirin therapy gives even better results than either alone-78% of patients report major symptom relief.
Regulatory agencies are stepping in too. The FDA released new safety guidelines for aspirin desensitization in 2023, standardizing protocols across clinics. Electronic tools like Penn Medicine’s AERD Management Toolkit are now used in over 40% of major hospitals, making it easier for doctors to follow best practices.
Telemedicine has helped bridge the access gap. Since 2020, remote consultations with AERD specialists have increased access by 35%. Still, only 18% of U.S. allergists feel confident managing AERD on their own. That’s why referral to a specialized center remains critical.
What Can Patients Do Every Day?
Managing AERD isn’t just about medications. Daily habits matter. Many patients in online communities swear by:
- Saline sinus rinses with a drop of tea tree oil to reduce fungal buildup
- Scheduling aspirin with meals to avoid stomach upset
- Reading labels on cold and pain meds-many contain hidden NSAIDs
- Using humidifiers in dry weather to keep nasal passages moist
Keeping a symptom diary helps track triggers and medication effects. And joining a patient group-like the AERD Warriors forum or Reddit’s r/SamtersTriad-can give you practical tips and emotional support.
What’s the Long-Term Outlook?
AERD is lifelong-but it doesn’t have to control your life. With proper management, most patients regain normal breathing, smell, and sleep. Those who undergo desensitization report the highest quality of life improvements. One study found 82% of desensitized patients said their sense of smell improved dramatically, compared to just 35% who didn’t.
Health economists estimate that integrated AERD care-surgery, desensitization, and biologics-can save $87,000 per patient over a lifetime by cutting hospital visits and surgeries. The key is early diagnosis and getting to a specialist before the disease becomes too advanced.
Can you outgrow Aspirin-Exacerbated Respiratory Disease?
No, AERD is a lifelong condition. It typically starts in adulthood and doesn’t go away on its own. Even if symptoms seem to improve, the underlying inflammation remains. Avoiding NSAIDs doesn’t stop progression. The only way to alter the disease course is through aspirin desensitization and long-term medical management.
Is aspirin desensitization safe for older adults?
Yes, age alone isn’t a barrier. Many patients over 60 have successfully completed desensitization. But doctors evaluate overall health carefully-especially heart and stomach conditions. If you have stable heart disease and no active ulcers, desensitization can still be a safe and effective option. The key is thorough screening and close monitoring during the procedure.
Can I take Tylenol (acetaminophen) if I have AERD?
Yes, acetaminophen is generally safe for people with AERD. Unlike aspirin or NSAIDs, it doesn’t strongly inhibit COX-1, so it doesn’t trigger the same inflammatory cascade. Many patients use Tylenol for pain or fever. However, high doses over long periods can still cause liver issues, so stick to recommended amounts.
Do I need to avoid all NSAIDs forever if I’m not desensitized?
Yes-if you haven’t gone through desensitization, you should avoid all COX-1 inhibitors, including ibuprofen, naproxen, diclofenac, and even some topical NSAIDs. Some people tolerate celecoxib (a COX-2 inhibitor) without issues, but this varies. Always check with your allergist before trying any new painkiller. Even small amounts can trigger a reaction.
How long does it take to feel better after aspirin desensitization?
Improvement isn’t instant. Most patients notice reduced nasal congestion and better breathing within 4 to 8 weeks of starting daily aspirin. Smell recovery takes longer-often 3 to 6 months. Asthma control usually improves within 2 months. The full benefits, like fewer polyp recurrences and less need for steroids, show up over 12 to 24 months. Patience and consistency are key.


Christina Widodo
I had no idea AERD was this complex. I thought it was just 'can't take ibuprofen' and called it a day. Learning about the leukotriene surge and how it literally rewrites your inflammation response blew my mind. This is why I love deep dives like this.