Joint Impact Calculator
Assess Your Joint Impact
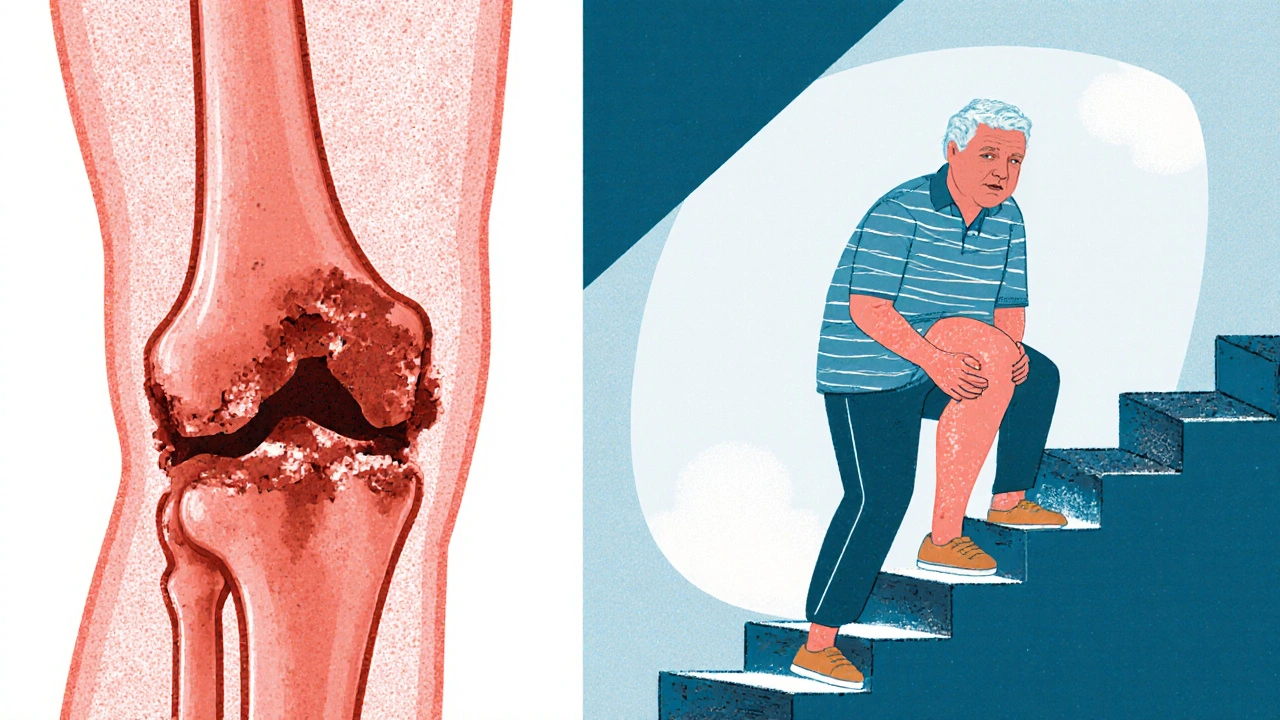
When you hear the term Joint Damage is the deterioration of cartilage, bone, ligaments, or tendons that connect two bones, leading to pain, stiffness, and reduced mobility. Whether it stems from injury, age‑related wear, or an autoimmune condition, the ripple effects reach far beyond the affected joint.
Key Takeaways
- Joint damage can cut work hours by up to 30 % and raise absenteeism risk.
- Daily activities like climbing stairs or carrying groceries become harder, affecting overall quality of life.
- Early intervention with therapy, ergonomic tweaks, and pain‑management plans can preserve career longevity.
- Legal protections such as disability benefits and workplace accommodations are available in many regions.
- Long‑term lifestyle changes-targeted exercise, nutrition, and weight control-slow further joint degeneration.
How Joint Damage Happens
Several pathways lead to a joint’s breakdown:
- Mechanical wear: Repetitive motions or heavy lifting gradually erode cartilage, especially in the knees and hips.
- Traumatic injury: A broken bone or ligament tear can trigger a cascade of inflammation that never fully heals.
- Inflammatory diseases: Conditions like rheumatoid arthritis cause the immune system to attack joint tissue.
- Metabolic factors: Obesity adds extra load, accelerating cartilage loss.
Three common diagnoses illustrate these causes:
| Condition | Primary Cause | Typical Age of Onset | Inflammation? | First‑Line Treatment |
|---|---|---|---|---|
| Osteoarthritis | Mechanical wear | 45‑65 | Low‑grade | Exercise + NSAIDs |
| Rheumatoid Arthritis | Autoimmune attack | 20‑50 | High‑grade | DMARDs + PT |
| Degenerative Joint Disease | Combined wear & metabolic | 60+ | Variable | Weight management + PT |
Career Consequences of Joint Damage
When a joint hurts, the whole workday feels off. A 2023 UK labour‑force study found that employees with chronic joint pain missed an average of 6 days per year, compared with 2 days for those without pain. Beyond absenteeism, presenteeism-being at work but less productive- can shave 15‑20 % off output.
Physical demands matter. Construction workers, nurses, and warehouse staff rely on lifting, bending, and prolonged standing. Even office workers aren’t immune; prolonged sitting can exacerbate hip or knee stiffness, while reaching for a keyboard places stress on the wrist.
Job titles most at risk include:
- Manual laborers (carpentry, plumbing)
- Healthcare providers (nurses, physiotherapists)
- Retail and warehouse staff
- Professional athletes and coaches
In contrast, careers that allow flexible positioning-software development, consulting, or remote administration-tend to offer more leeway for ergonomic adaptations.

Lifestyle Ripples Outside the Office
Joint damage seeps into everyday moments. Climbing stairs, gardening, or simply walking the dog can become mini‑obstacles. This loss of independence often triggers emotional stress, with a 2022 meta‑analysis linking chronic joint pain to a 30 % higher odds of depression.
Social activities may decline as well. Invitations to dance, hikes, or sports become less appealing, leading to a more sedentary lifestyle-a paradox that further damages joints.
Sleep quality suffers too. Night‑time pain forces many to adopt awkward sleeping positions, resulting in fragmented rest and daytime fatigue, which compounds work‑related performance issues.
Managing Pain and Treatment Options
Effective pain control starts with a multi‑modal approach. Over‑the‑counter NSAIDs help for occasional flare‑ups, but long‑term reliance raises gastrointestinal and cardiovascular risks.
Targeted therapies include:
- Physical Therapy: Tailored exercises improve strength, preserve range of motion, and teach joint‑protective techniques.
- Occupational Therapy: Focuses on adapting daily tasks and workstations to reduce strain.
- Injectable treatments (corticosteroids, hyaluronic acid) for short‑term relief.
- Prescription disease‑modifying drugs for inflammatory forms like rheumatoid arthritis.
- Joint Replacement Surgery: Offers lasting relief for end‑stage osteoarthritis when conservative measures fail.
Beyond medical options, lifestyle tweaks-maintaining a healthy weight, low‑impact cardio (swimming, cycling), and a diet rich in omega‑3 fatty acids-slow cartilage breakdown. Cartilage health benefits from nutrients like glucosamine and chondroitin, though evidence varies.
Workplace Adjustments and Legal Rights
Employers are increasingly aware of the need for ergonomic solutions. A well‑designed workstation-adjustable chairs, sit‑stand desks, and monitor arms-reduces strain on the lumbar spine, shoulders, and wrists.
Workplace Ergonomics can prevent further joint damage and boost productivity. Simple steps include:
- Positioning keyboard and mouse at elbow height to keep wrists neutral.
- Using a footrest to maintain proper hip angle.
- Implementing micro‑breaks every 30 minutes to stand or stretch.
In the UK, the Equality Act 2010 obliges employers to provide reasonable adjustments for employees with a disability, which includes chronic joint conditions. This may involve modified duties, flexible hours, or assistive devices.
When adjustments aren’t enough, Disability Benefits such as Employment and Support Allowance (ESA) or Personal Independence Payment (PIP) can supplement income while you manage your health.

Long‑Term Planning and Lifestyle Adaptation
Think of joint health as a marathon, not a sprint. Regular check‑ups with a rheumatologist or orthopaedic specialist help track disease progression.
Adopt a weekly routine that blends:
- Low‑impact cardio (e.g., 30 minutes of swimming, 3 times a week).
- Strength training focused on muscles supporting the affected joint.
- Flexibility work- yoga or gentle stretching-to maintain range of motion.
- Mind‑body practices like meditation, which lower perceived pain levels.
When symptoms flare, have a pre‑planned action kit: pain‑relief medication, ice pack, and a quick‑access list of supportive contacts (therapist, employer HR rep, doctor).
Checklist: Evaluate and Act on Joint‑Damage Impact
- Identify the affected joint(s) and record pain patterns.
- Consult a healthcare professional for diagnosis (OA, RA, etc.).
- Discuss treatment options-therapy, medication, surgery.
- Request an ergonomic assessment at work.
- Explore legal protections and possible disability benefits.
- Implement a tailored exercise and nutrition plan.
- Schedule regular follow‑ups to monitor progress.
Frequently Asked Questions
Can joint damage be reversed?
Complete reversal is rare, but early treatment can halt or even improve symptoms. Strengthening the surrounding muscles and reducing inflammation often leads to noticeable functional gains.
What jobs are safest for someone with osteoarthritis?
Roles that allow frequent movement, sitting, and minimal heavy lifting-such as administrative work, remote IT, or consulting-tend to be safest. Adjustments like sit‑stand desks further reduce risk.
How much does joint replacement surgery cost in the UK?
For NHS patients, the procedure is free at the point of use. Private surgery averages £9,000 - £13,000 per joint, depending on hospital and surgeon.
Are there specific foods that help protect joints?
Foods rich in omega‑3 fatty acids (salmon, walnuts), antioxidants (berries, leafy greens), and vitamin D (fortified milk, sunlight exposure) support cartilage health and reduce inflammation.
What legal rights do I have if my employer can’t accommodate my joint condition?
Under the Equality Act 2010, an employer must make reasonable adjustments. If they fail, you can raise a formal grievance, seek mediation, or pursue an employment tribunal claim.

Sarah Hanson
Thanks for putting together such a thorough overview of joint damage and its impact. I'll definitely be sharing this with my rehab team.