Immunosuppression Therapy Monitoring Tool
Calculate Your Monitoring Status
Enter your current immunosuppressant levels and TTV results to see if you're in the safe range for both rejection and infection risk.
Key Information
For tacrolimus, target range is 5-10 ng/mL in first 3 months, then 3-7 ng/mL. For TTV, safe range is 2.5-3.5 log10 copies/mL. Levels outside these ranges increase rejection or infection risk.
When you're on immunosuppressive drugs-whether after a kidney transplant, for lupus, or another autoimmune condition-you're walking a tightrope. Too much drug, and your body can't fight off infections. Too little, and your immune system attacks your new organ or your own tissues. That’s why monitoring during immunosuppressive therapy isn’t optional. It’s life-saving.
Why Monitoring Isn’t Just a Routine Checkup
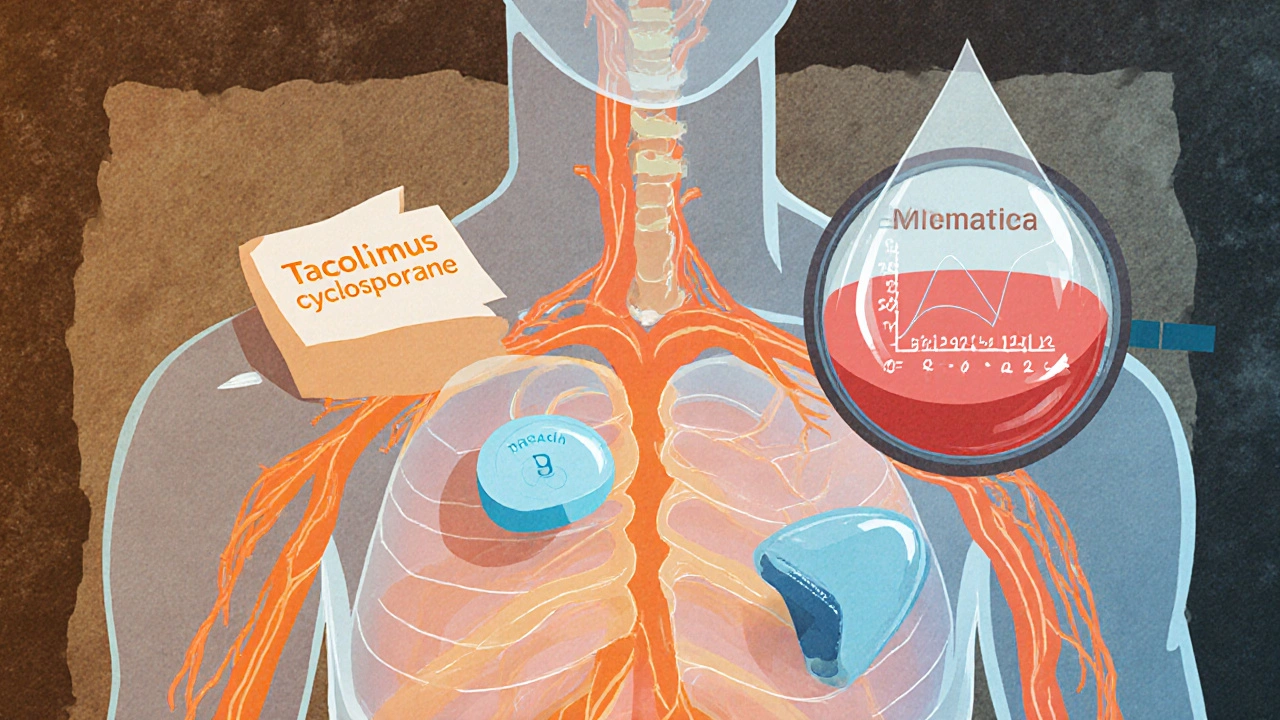
Immunosuppressants like tacrolimus, cyclosporine, and mycophenolate aren’t like regular pills. A small change in your blood level can mean the difference between a healthy transplant and rejection. These drugs have what’s called a narrow therapeutic index. That means the gap between the dose that works and the dose that harms you is tiny. Two people taking the same pill, at the same dose, can have wildly different blood levels-one safe, the other toxic. This isn’t guesswork. In 2021, the American Journal of Transplantation confirmed that patients who had their drug levels checked regularly had 37% fewer acute rejections and 22% better five-year graft survival than those on fixed doses. That’s not a small benefit. That’s the difference between living five more years and losing your transplant.Therapeutic Drug Monitoring: The Cornerstone of Care
The most critical part of monitoring is therapeutic drug monitoring (TDM). Not all immunosuppressants need it, but the big ones do.- Tacrolimus: Target levels are 5-10 ng/mL in the first 3 months after transplant, then dropped to 3-7 ng/mL. Levels are checked at trough-just before your next dose. Missing this window can mean underdosing, which raises rejection risk.
- Cyclosporine: Often monitored with both trough (C0) and 2-hour post-dose (C2) levels. C2 is more accurate at predicting rejection. If your C2 is too low, your body might be rejecting the organ-even if your trough looks fine.
- Sirolimus and Everolimus: Target range is 5-10 μg/L, but guidelines are weaker here. Some centers don’t monitor routinely because the link between levels and outcomes isn’t as clear.
- Mycophenolic acid (MPA): Tricky. Because of how it’s processed in the gut, trough levels don’t tell the full story. The best measure is AUC-the total drug exposure over 12 hours. An AUC of 30-60 mg·h/L is linked to 85% rejection-free survival in the first year.
What Blood Tests You Need Every Few Months
Beyond drug levels, routine labs catch the side effects before they become emergencies.- Renal function: Creatinine and urea. Cyclosporine and tacrolimus are kidney-toxic. A 30% rise in creatinine from baseline happens in 1 in 4 patients. Catching it early can prevent permanent damage.
- Electrolytes: Magnesium drops in 40-60% of cyclosporine users. Low magnesium causes muscle cramps, irregular heartbeat, and seizures. It’s easily fixed with supplements if caught.
- Full blood count: Mycophenolate causes low white blood cells (leukopenia) in 25-30% of patients, low platelets in 10-15%. That means higher infection and bleeding risk. Monthly checks are standard in the first year.
- Liver enzymes: All these drugs stress the liver. AST and ALT spikes mean you might need a dose adjustment.
- Lipids and glucose: Sirolimus raises cholesterol in 60-75% of patients. Tacrolimus increases diabetes risk by 30% compared to other drugs. Fasting lipids and glucose are checked every six months.
- Calcium, phosphate, uric acid: These can go haywire with long-term use, especially with steroids. High uric acid means gout. Low calcium means bone loss.
Imaging: Seeing What Blood Tests Can’t
Some problems don’t show up in bloodwork. That’s where imaging comes in.- Renal ultrasound: Done annually or if creatinine rises. Checks for blockages, fluid around the kidney, or signs of chronic damage. It’s quick, safe, and non-invasive.
- Chest X-ray: If you have a cough, fever, or shortness of breath, this is the first step. Sirolimus can cause pneumonitis-a rare but serious lung inflammation. X-rays catch it in 70-85% of cases.
- Bone density scan (DEXA): Steroids eat away at bone. After one year of steroid therapy, you need a baseline scan. Then every year. Osteoporosis is silent until you break a hip. Prevention is far easier than repair.
The Future Is in Your Virus: TTV Monitoring
Here’s one of the most exciting advances: Torque Teno Virus (TTV) monitoring. TTV is a harmless virus that infects almost everyone. In healthy people, your immune system keeps it in check. But when you’re immunosuppressed, TTV multiplies like crazy. The amount of TTV in your blood directly reflects how suppressed your immune system is. Studies show:- TTV levels below 2.5 log10 copies/mL = high rejection risk (3.2 times more likely)
- TTV levels above 3.5 log10 copies/mL = high infection risk (2.7 times more likely)
- The ideal range? 2.5-3.5 log10 copies/mL for months 4-12 after transplant.
What’s Holding Back Better Monitoring?
Even with all this science, real-world practice is messy. A 2022 survey of 150 transplant centers found:- 68% had inconsistent TDM protocols between different teams in the same hospital.
- Only 42% had standardized methods for MPA monitoring.
- 75% said cost was the biggest barrier.
- 63% lacked clear reference ranges for newer drugs.
What’s Next? AI, Point-of-Care Tests, and Breath Analysis
The future is smarter, faster, and less invasive.- AI prediction models: A 2023 study in Nature Medicine built an algorithm that predicted transplant rejection 14 days before symptoms appeared-by analyzing patterns in tacrolimus levels, TTV, and lab values. Accuracy? 87%.
- Point-of-care TDM devices: Imagine getting your tacrolimus level checked in the clinic with a finger-prick, like a glucose meter. Several are in phase 2 trials. FDA approval is expected by 2026-2027.
- Exhaled breath analysis: Researchers are testing whether immunosuppressant metabolites can be detected in your breath. Still early, but if it works, it could replace blood draws entirely.
Is All This Monitoring Worth It?
Yes. A 2022 cost analysis found that full monitoring adds $2,850 per patient per year-but saves $8,400 by preventing hospital stays, rejections, and infections. That’s a return of nearly $3 for every $1 spent. And it’s not just about transplants anymore. Autoimmune diseases like rheumatoid arthritis, MS, and Crohn’s are using these same drugs. As their use expands, monitoring will become even more critical. The goal isn’t just to keep you alive. It’s to keep you well. To let you live without constant fear of rejection or infection. To give you back your life.That’s what monitoring does. It’s not just science. It’s care.
How often do I need blood tests while on immunosuppressants?
In the first year after transplant or starting therapy, you’ll likely need blood tests every 1-2 weeks. After that, it tapers to every 2-4 weeks, then monthly or every 2-3 months if your levels are stable. The exact schedule depends on your drug, how long you’ve been on it, and your overall health. Always follow your care team’s plan-don’t skip tests just because you feel fine.
Can I stop monitoring if I’ve been stable for years?
No. Even if you’ve been stable for 5 or 10 years, your body changes. Your kidneys age, your metabolism shifts, you might start new medications, or develop an infection. These all affect how your body handles immunosuppressants. Stopping monitoring increases your risk of late rejection or drug toxicity. Most experts recommend lifelong, though less frequent, monitoring.
Why does my doctor check magnesium and not just my drug levels?
Cyclosporine and tacrolimus cause your body to lose magnesium through the kidneys. Low magnesium isn’t just a side effect-it makes your drugs less effective and can cause dangerous heart rhythms or muscle spasms. Checking magnesium is like checking your fuel gauge. Even if your drug level looks right, low magnesium can still trigger rejection. It’s a hidden piece of the puzzle.
Is TTV monitoring available everywhere?
Not yet. TTV testing is still mostly in research centers and major transplant hospitals. It’s not FDA-approved for routine use in the U.S. as of 2025, though it’s being used off-label in some places. The TTVguideIT trial results, expected in 2026, could change that. Ask your transplant team if they’re participating in TTV studies or plan to offer it soon.
What should I do if my drug level is too high?
Don’t stop your medication or change your dose on your own. A high level means you’re at risk for kidney damage, nerve problems, or infections. Your doctor may lower your dose, switch drugs, or delay your next dose. They’ll also check for interactions-like grapefruit juice or certain antibiotics-that can spike levels. Always report new symptoms like tremors, nausea, or swelling.
Can I reduce my monitoring if I’m on steroids only?
Not really. While steroids don’t need TDM, they still require regular monitoring for blood sugar, bone density, blood pressure, and eye health. Long-term steroid use can cause diabetes, cataracts, osteoporosis, and high blood pressure. Monitoring is just as important-even if the tests are different.

Brittney Lopez
Just wanted to say how much I appreciate posts like this-clear, detailed, and actually helpful. I’m a nurse in a transplant clinic, and this is exactly what I tell patients when they’re overwhelmed. You’re not just checking numbers; you’re protecting their future. Thank you for putting this together.