Since 2018, a quiet but dangerous problem has shaken the generic drug industry: nitrosamine contamination. These aren’t just chemical byproducts-they’re potent carcinogens found in pills millions of people take every day. What started with a single recall of valsartan for high blood pressure quickly spread to metformin, ranitidine, duloxetine, and even varenicline. By mid-2025, the FDA had issued over 500 recalls tied to nitrosamines. For patients, it’s not just about missing a prescription-it’s about trusting that the medicine in your bottle won’t hurt you over time.
What Are Nitrosamines and Why Do They Matter?
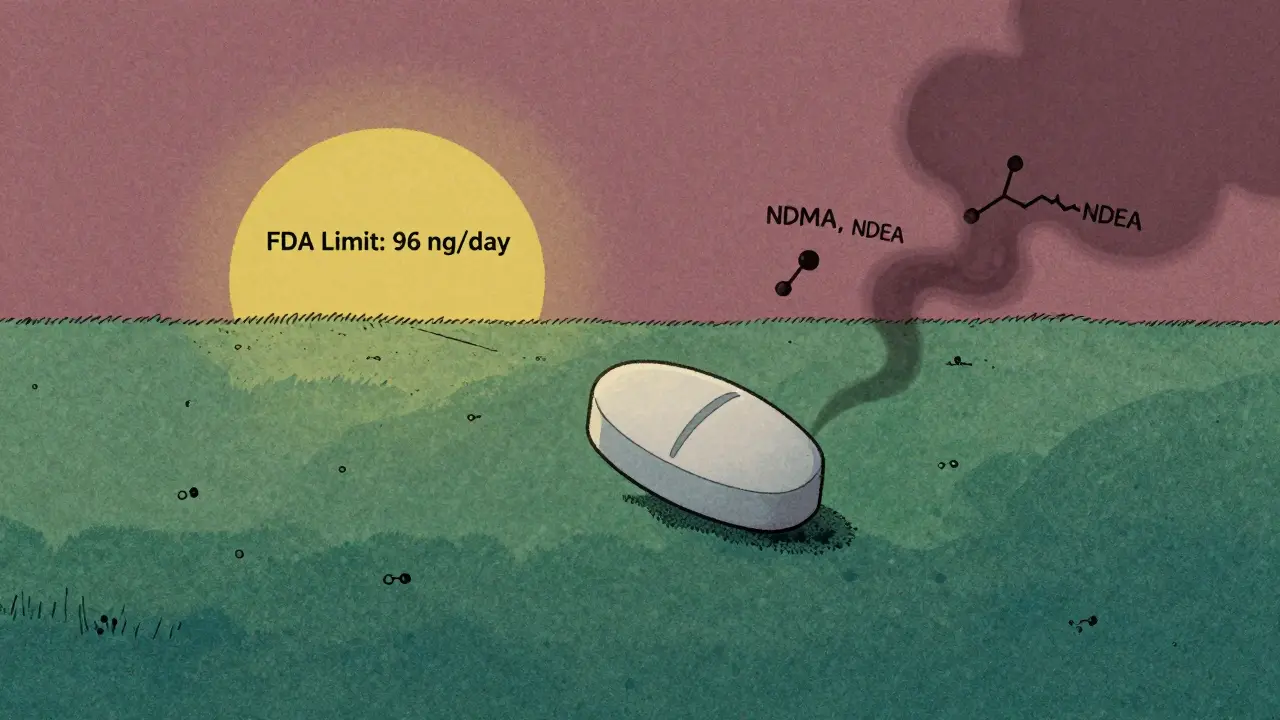
Nitrosamines are a group of chemicals that form when certain amines react with nitrites under heat, pressure, or specific pH conditions. They’re not added on purpose. They sneak in during manufacturing, packaging, or even storage. The most common ones found in drugs are NDMA (N-Nitrosodimethylamine), NDEA (N-Nitrosodiethylamine), and newer compounds called NDSRIs-like N-nitroso-varenicline and N-nitroso-duloxetine.
The FDA classifies them as probable human carcinogens. That means even tiny amounts, measured in nanograms per day, can increase cancer risk over years of exposure. For context: one nanogram is one billionth of a gram. The acceptable daily intake for NDMA is 96 ng/day. That’s less than the weight of a single grain of salt spread across your entire daily dose of medication.
It’s not about acute poisoning. It’s about long-term, low-level exposure. A person taking contaminated metformin for 10 years might never feel sick-but their cancer risk could rise slightly. That’s why regulators treat this like a silent public health threat.
How Did This Happen? The Recalls That Changed Everything
The first major wake-up call came in July 2018, when the FDA announced that some batches of valsartan-used to treat high blood pressure and heart failure-contained NDMA. The source? A change in the manufacturing process at a supplier in China. Within weeks, similar contamination was found in losartan and irbesartan. By the end of 2019, over 10 products had been pulled from U.S. shelves.
Then came ranitidine (Zantac). The popular heartburn drug was taken off the market in 2020 after it was found to form NDMA over time, even in sealed bottles. The issue wasn’t just manufacturing-it was instability. The molecule itself broke down into nitrosamines during shelf life.
By 2023, the list grew: metformin for diabetes, duloxetine for depression and nerve pain, varenicline for smoking cessation. Each recall had a different root cause. One manufacturer found nitrites in magnesium stearate-a common excipient-from a single supplier. Another discovered that blister pack adhesives released amines that reacted with nitrites in the air inside the package.
By mid-2025, the FDA had recorded over 40 specific drug product recalls directly linked to nitrosamines. But the real number is higher. Many manufacturers voluntarily test and reformulate without public recalls, especially if they catch the issue early.
What’s the FDA Doing Now? Rules, Deadlines, and Flexibility
The FDA’s response has been aggressive but evolving. In 2023, they released detailed guidance on acceptable intake limits for each nitrosamine. For NDEA, it’s 26.5 ng/day. For most NDSRIs, it’s 96 ng/day. But here’s the catch: if a drug contains more than one nitrosamine, the limits aren’t additive. If two impurities are each at 80% of their individual limits, you’re already over the safety threshold.
In September 2024, the FDA made testing requirements even stricter. Manufacturers now need to use highly sensitive LC-MS/MS methods capable of detecting nitrosamines at 0.3 to 3 ng/mL. That’s like finding a single drop of ink in an Olympic-sized swimming pool.
Then came the August 1, 2025 deadline for full compliance with NDSRI controls. But in June 2025, the FDA quietly changed course. Instead of requiring full reformulation by that date, they now accept detailed progress reports. Companies must still act-they just don’t have to finish by August.
This wasn’t a retreat. It was a recognition of reality. One mid-sized generic maker spent $2 million and 18 months just fixing nitrosamine issues in their metformin line. Another took 14 months to switch suppliers after finding nitrite contamination in magnesium stearate. The FDA admitted: “Nitrosamine mitigation strategies vary widely and can demand extensive time and supply-chain adjustments.”
Who’s Getting Hit the Hardest?
It’s not just big companies. Small and mid-sized generic manufacturers are under the most pressure. They often lack in-house analytical labs, regulatory teams, or the cash reserves to revalidate entire production lines.
Tea and Fresenius Kabi, with global supply chains and deep pockets, have built robust nitrosamine control programs. They test every batch. They audit suppliers. They redesign packaging. Smaller players? Many are still struggling. Some have stopped making certain older generics because the cost of compliance exceeds the profit.
That’s led to shortages. Between 2018 and 2020, 15-20% of ARB products were temporarily unavailable. Patients had to switch brands, sometimes to ones they’d never tried before. Pharmacists had to explain why their usual prescription was gone-and why the replacement might cost more.
According to Evaluate Pharma’s 2025 analysis, nitrosamine compliance has cut generic drug profit margins by 3-5 percentage points. That’s not just a line item-it’s forcing consolidation. Smaller firms are being bought out. Others are exiting the market entirely.
What Are Manufacturers Doing to Fix This?
Successful companies didn’t wait for the FDA to act. They started testing early. They looked beyond the active ingredient. They asked: What’s in the filler? The coating? The bottle? The adhesive on the blister pack?
One manufacturer found that changing from a secondary amine-based blister film to a polyethylene-based one eliminated a major nitrosamine pathway. Another replaced sodium nitrite in a cleaning step with a non-nitrosating alternative. Some switched to nitrogen-purged packaging to remove oxygen and prevent reactions.
But it’s not always that simple. Fixing one problem often creates another. One company reduced NDMA by changing solvent use-only to find NDEA popping up in a different batch. They had to go back, retest, and revalidate again. It’s a game of whack-a-mole, with cancer risk on the line.
Companies that succeeded did three things: they invested in analytical capability, they mapped every possible formation pathway, and they worked closely with suppliers. Nitrosamines don’t care if you’re a big pharma giant or a small lab. They form wherever amines and nitrites meet under the right conditions.

What This Means for Patients
Should you stop taking your generic medication? No. The FDA and other regulators emphasize that the cancer risk from trace nitrosamines is low-especially compared to the risks of not treating conditions like hypertension, diabetes, or depression.
But you should know: if your prescription suddenly changes brand or manufacturer, it might be because of nitrosamine reformulation. That’s not a red flag-it’s a sign the system is working. The new version is likely safer.
If you’re concerned, talk to your pharmacist. Ask: “Has this medication been affected by any recalls?” Most pharmacists can check the FDA’s recall database. You can also search the FDA’s website directly for your drug name and “nitrosamine.”
Don’t panic. But don’t ignore it either. This isn’t a one-time event. It’s a new standard in drug safety. The bar has been raised-and it’s not coming down.
What’s Next?
The FDA has signaled that nitrosamine testing will expand to more drug classes. Antivirals, antifungals, and even some antibiotics are now on the radar. Packaging materials are getting stricter scrutiny. Even the ink on pill coatings is being tested.
Expect more recalls. More reformulations. More delays in generic approvals. But also expect better, safer medicines in the long run. The cost is high-for manufacturers, for regulators, and for patients who pay more or wait longer. But the alternative-ignoring carcinogens in daily pills-is unthinkable.
Generic drugs saved the U.S. healthcare system hundreds of billions of dollars. Now, they’re being held to a higher standard. And that’s a good thing.
Are nitrosamines only found in generic drugs?
No. Nitrosamines can form in any drug-brand-name or generic-where the manufacturing process or ingredients allow it. But they’ve been more common in generics because many manufacturers use lower-cost suppliers, older processes, or simplified formulations that are more vulnerable to contamination. Brand-name companies often have tighter controls from the start, but recalls have also happened in branded products like Zantac (ranitidine).
How do I know if my medication is safe?
Check the FDA’s drug recall database using your drug’s name and the word “nitrosamine.” Your pharmacist can also help. If your prescription was recently switched to a different manufacturer or generic version, it may have been changed to meet new safety standards. Don’t assume an older batch is safe-some drugs form nitrosamines over time, even in sealed bottles.
Can I test my pills at home for nitrosamines?
No. Detecting nitrosamines requires advanced lab equipment like liquid chromatography-tandem mass spectrometry (LC-MS/MS), which can measure parts per billion. Home test kits don’t exist for this purpose. If you’re worried, contact your pharmacist or doctor-they can help determine if your medication has been recalled or reformulated.
Why did the FDA delay the August 2025 deadline?
The FDA realized that many manufacturers, especially smaller ones, needed more time to identify root causes, redesign processes, and gather stability data. Reformulating a drug isn’t like changing a recipe-it requires full revalidation, new testing protocols, and regulatory submissions. The delay wasn’t a relaxation of standards-it was an acknowledgment that fixing this problem takes time, resources, and careful science.
Is it safe to keep taking my generic metformin or valsartan?
Yes-if it hasn’t been recalled. The cancer risk from trace nitrosamines is very low, especially compared to the risks of uncontrolled diabetes or high blood pressure. The FDA advises patients to continue taking their medication unless told otherwise by their doctor. If your drug was recalled, your pharmacist will provide a replacement. Don’t stop taking it without medical advice.

Jim Rice
This whole nitrosamine thing is a scam. If you’re worried about nanograms of carcinogens in your pills, you’re the same person who buys organic kale at $12 a bag and thinks WiFi gives you cancer. The real risk? Not taking your blood pressure med and having a stroke. Grow up.