Every time you pick up a prescription, there’s a small sticker on the bottle that could save your life-or hurt you if you ignore it. These aren’t just random notes from the pharmacist. They’re legally required safety messages, designed to stop dangerous mistakes before they happen. But here’s the problem: most people don’t understand what they really mean.
What Those Stickers Are Really For
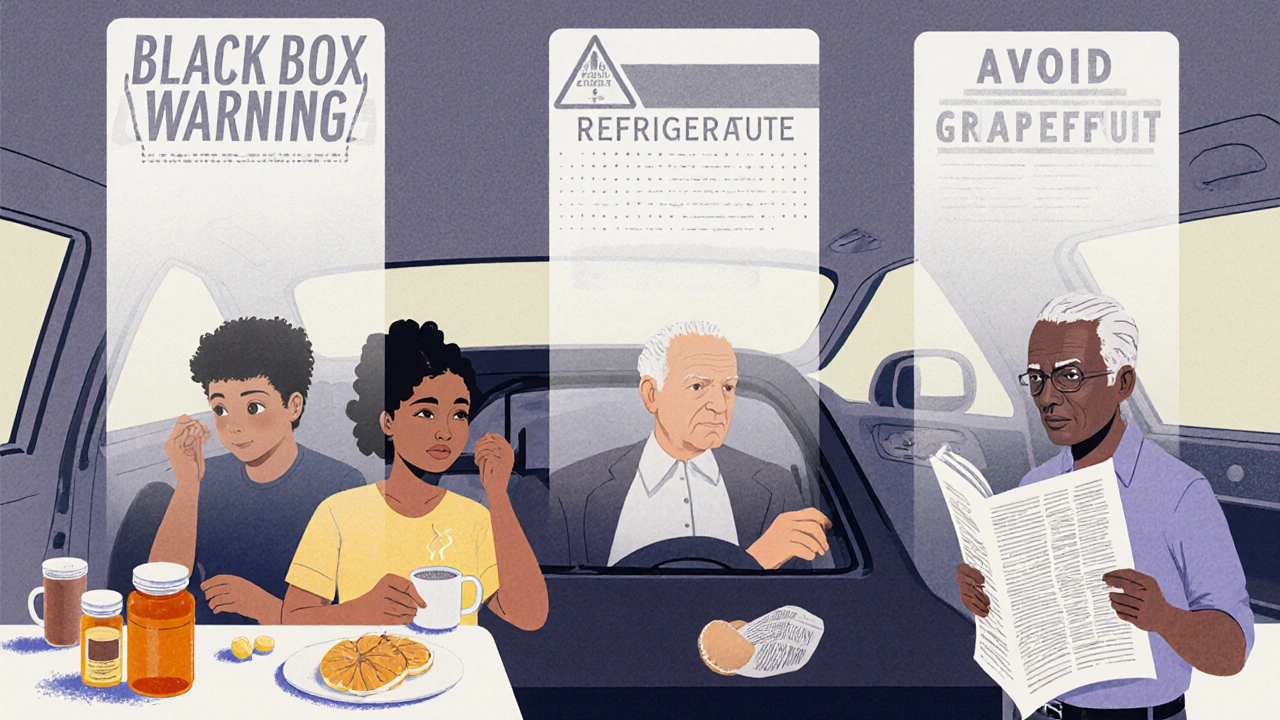
Those little colored stickers on your pill bottle aren’t decoration. They’re part of a federal safety system enforced by the FDA. Under the Federal Food, Drug, and Cosmetic Act, every prescription must carry warnings that prevent injury. These aren’t suggestions. They’re rules. The FDA estimates that if everyone understood their labels correctly, 30 to 50% of harmful drug reactions could be avoided each year. That’s over a million injuries prevented annually.The most serious warnings are called Black Box Warnings. These are printed in bold, with a thick black border around them, and appear at the top of the prescribing info. They’re used when a drug has been linked to life-threatening side effects-like liver failure, heart rhythm problems, or suicidal thoughts. About 40% of new drugs approved between 2013 and 2017 carried one. If your medication has this, it doesn’t mean you can’t take it. It means you need to know the risks and watch for warning signs.
Color Matters-But Not How You Think
You’ve probably noticed red, yellow, blue, and white stickers. Many people assume red means "danger," yellow means "caution," and the rest are just reminders. That’s mostly true. A study in U.S. Pharmacist found that 85% of patients correctly understood red labels as "immediate danger," while only 45% got the meaning of blue ones. But here’s the catch: not all pharmacies use the same colors. Some use red for "take with food," others for "avoid alcohol." There’s no national standard for color coding yet.That’s why you can’t rely on color alone. Always read the words. A red sticker that says "Do not crush" is more important than a yellow one that says "Take in the morning." The color draws your eye, but the text tells you what to do.
Common Warnings-and What They Actually Mean
Some warnings sound simple, but people get them wrong all the time.- "Take on empty stomach" means at least one hour before or two hours after eating. Food can block absorption. If you take your thyroid medicine with coffee or cereal, it won’t work.
- "Take with food" isn’t about comfort-it’s about safety. Some drugs irritate your stomach lining. Taking them on an empty stomach can cause ulcers or bleeding. A Healthline survey found 42% of people ignore this, thinking it’s optional.
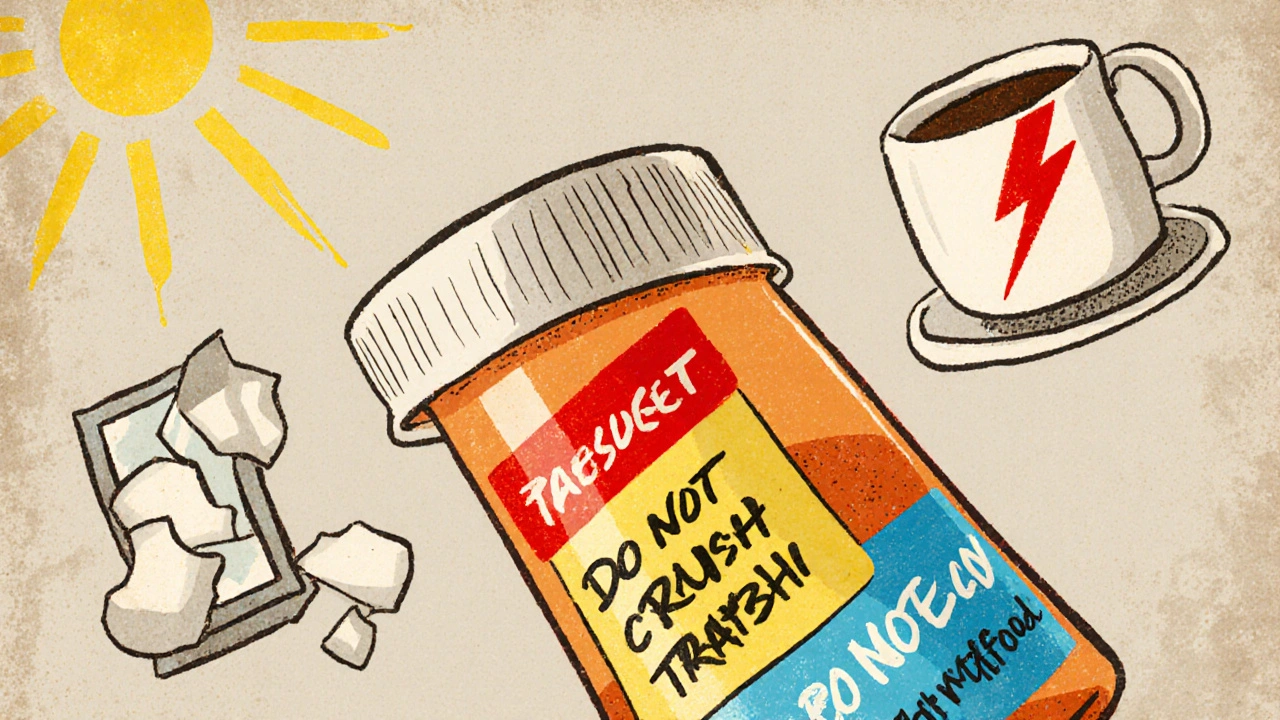
- "Do not crush or chew" is often misunderstood. People think "don’t crush" means "don’t chew it up," but it actually means: swallow the whole pill. Crushing or chewing can release the full dose at once, causing overdose. One study showed 30% of patients misread this as "chew thoroughly."
- "Refrigerate" means keep it between 36°F and 46°F. Not just "keep it cool." If you leave insulin or certain antibiotics out, they lose potency. You won’t feel sick right away-but the drug won’t work when you need it.
- "Avoid sunlight" doesn’t just mean don’t tan. Some drugs make your skin burn easily-even through windows. One patient on Drugs.com ended up in the ER after taking a blood pressure med and getting sunburned through her kitchen window.
- "Do not operate heavy machinery" includes driving, using power tools, or even climbing ladders. If the drug causes drowsiness, dizziness, or blurred vision, you’re at risk of falling or crashing. A Kaiser Permanente patient said this warning kept them from getting into a car accident after starting a new anxiety medication.
Why You Keep Missing the Warnings
You’re not lazy. You’re just overwhelmed. Studies show the average person spends just 7 to 12 seconds looking at their prescription label. That’s less time than it takes to read this sentence. And if the label is printed in tiny font on a curved bottle? Good luck.Even worse, most people throw away the printed Patient Prescribing Information (PPI) sheet that comes with the pill bottle. A 2020 study found 68% of patients toss it out, thinking it’s just paperwork. But that sheet has the full details-drug interactions, rare side effects, what to do if you miss a dose. It’s not junk mail. It’s your safety manual.
Another problem? Health literacy. The National Assessment of Adult Literacy found only 12% of U.S. adults have proficient health literacy. That means 88% struggle to understand medical terms like "contraindication," "adverse reaction," or "bioavailability." When a label says "avoid grapefruit juice," and you don’t know what grapefruit juice does to your liver enzymes, you just think, "I like grapefruit. I’ll take my chances."
What’s Being Done to Fix This
The system isn’t broken-it’s outdated. The FDA started pushing for change in 2022 with its "Facts Label" initiative. Starting in June 2025, 20 high-risk drug classes-including blood thinners, diabetes meds, and opioids-must use simplified, easy-to-read labels with plain language and standardized icons.One new icon? A slashed pill with a hammer over it. That means "do not crush." In testing, this symbol reduced misinterpretation from 31% to just 8%. Another pilot program lets pharmacies put QR codes on labels. Scan it, and you get a 60-second video from your pharmacist explaining the warning in plain English. Mayo Clinic trials showed this boosted understanding by 52%.
Some pharmacies are already ahead of the curve. Walgreens’ "Medication Safety Check" program includes a 5-minute one-on-one review with a pharmacist. Patients who went through it had 92% comprehension of their warnings. Independent pharmacies without this service? Only 68%.

How to Actually Understand Your Labels
You don’t have to wait for the system to fix itself. Here’s how to protect yourself today:- Match the pill to the label. Check the shape, color, and imprint code (the letters or numbers on the pill). If it doesn’t match what’s on the bottle, ask the pharmacist. Pills can be switched accidentally.
- Read the sticker out loud. Don’t just glance. Say it. If you can’t explain it in your own words, you don’t understand it.
- Use the "teach-back" method. After the pharmacist gives you instructions, say: "So, just to make sure I got this right-I take this with food because it upsets my stomach, and I can’t drink grapefruit juice. Is that correct?" This simple trick improves understanding by 47%.
- Keep the PPI sheet. Tape it to your fridge or stick it in your wallet. You’ll need it when you see a new doctor or get a refill.
- Ask about interactions. If you take supplements, herbal teas, or over-the-counter painkillers, ask: "Will this interact with my new prescription?" Many people don’t realize that St. John’s Wort can cancel out birth control or that ibuprofen can make blood thinners dangerous.
The Bottom Line
Prescription labels aren’t meant to confuse you. They’re meant to protect you. But the system was built for doctors, not patients. Until the FDA’s new rules fully roll out in 2025 and 2026, you have to be your own safety net.Don’t assume you know what a warning means. Don’t trust color alone. Don’t throw away the paper. And if something feels unclear-ask. Again. And again. Your pharmacist isn’t there to rush you. They’re there to keep you alive.
What does a black box warning on a prescription mean?
A black box warning is the strongest safety alert the FDA requires. It means the drug has been linked to serious, possibly life-threatening side effects-like organ failure, heart problems, or suicide risk. It doesn’t mean you can’t take the drug, but you need to know the signs of trouble and report them right away. Your doctor and pharmacist should explain this warning before you start taking it.
Why do some pills say "do not crush"?
"Do not crush" means the pill is designed to release the medicine slowly over time. Crushing or chewing it releases the full dose all at once, which can cause overdose. This is common with extended-release painkillers, blood pressure meds, and ADHD drugs. Even if the pill tastes bad or is hard to swallow, swallow it whole. If you can’t, ask your doctor for a liquid version.
Is it safe to ignore "take with food" if I forget?
No. "Take with food" is often about preventing serious side effects like stomach bleeding or nausea. Some drugs, like antibiotics or steroids, can damage your stomach lining if taken empty. If you forget, take it as soon as you remember-with a snack or meal. Don’t wait until your next dose. Skipping food increases your risk of harm.
Can I rely on the color of the warning sticker?
No. While red often means "danger" and yellow means "caution," there’s no national standard. One pharmacy might use red for "avoid alcohol," another for "take at bedtime." Always read the words. Color helps you notice the sticker-but the text tells you what to do.
What should I do if I don’t understand a warning?
Ask your pharmacist to explain it in plain language. Don’t say "I don’t get it." Say: "Can you tell me what this means for me?" Then repeat it back: "So, this means I can’t drink grapefruit juice because it makes my medicine too strong?" This "teach-back" method ensures you really understand. If they’re busy, call back later. Your safety matters more than their schedule.
Are warning labels the same everywhere in the U.S.?
No. There are over 3,500 different labeling systems used by community pharmacies across the country. That’s why the same drug might have different stickers at CVS, Walgreens, and your local independent pharmacy. The FDA is working to standardize labels by 2026, but until then, always check with your pharmacist and keep your written instructions.
Why do I get different warning stickers when I refill the same prescription?
That’s usually because your prescription was filled by a different pharmacy or the manufacturer changed the label. Sometimes, the drug maker updates the safety info, and the new label reflects it. Always compare the new sticker to the old one. If anything changed-especially a red or black box warning-call your pharmacist and ask why.

Barry Sanders
This is why people die from meds. Not because they’re dumb-because the system is designed to confuse them. That red sticker? Could mean ‘don’t drink’ or ‘take at night’ depending on which pharmacy you hit. No standard. No accountability. Just luck.