Why Medication Guides Matter More Than You Think
Every time you pick up a new prescription, you get a small paper insert-sometimes tucked in the box, sometimes handed to you at the counter. It’s easy to ignore. But if you skip reading it, you could be missing life-saving information. These aren’t just instructions. They’re medication guides, legally required by the FDA for drugs with serious, preventable risks. Think of them as your personal safety checklist for what could go wrong-and how to stop it before it happens.
Unlike general drug labels, medication guides focus on the big dangers: liver damage, blood disorders, suicidal thoughts, internal bleeding. They don’t sugarcoat. They say exactly what to watch for, when to get tested, and when to call your doctor right away. And they’re written to be understood-not by doctors, but by you.
What’s Inside a Medication Guide (and Where to Find the Critical Parts)
Every FDA-approved medication guide follows the same seven-section format. You don’t need to read every word, but you do need to know where to find the parts that matter most.
- “What is the most important information I should know about [drug name]?” This is your first stop. It’s where the FDA forces manufacturers to spell out the top risks in plain language. No jargon. No fluff. If a drug can cause sudden liver failure or a deadly drop in white blood cells, this section says it outright.
- “What should I tell my healthcare provider before taking [drug name]?” This tells you what conditions or medications could make your prescription dangerous. For example, if you have a history of liver disease, some drugs here will say: “Don’t take this.”
- “What are the possible or reasonably likely serious side effects of [drug name]?” This is where monitoring advice lives. Look for phrases like “get your blood tested regularly,” “check your INR every month,” or “call your doctor immediately if you notice…” These aren’t suggestions-they’re requirements.
- “How should I take [drug name]?” This section often includes timing for tests. “Your provider should test your blood before you start and every 3 months after.” That’s not vague. That’s a schedule.
For example, the guide for warfarin (Coumadin) doesn’t just say “watch for bleeding.” It says: “If you notice unusual bruising, nosebleeds that won’t stop, or red or black stools, call your doctor right away. Your INR must be checked at least once a month-and more often if your dose changes.” That’s specific. That’s actionable.
How to Spot the Red Flags in the Text
Not all warning language is created equal. Some phrases are code for serious risk. The Agency for Healthcare Research and Quality (AHRQ) has identified seven key red flags you should underline the moment you see them:
- “Get blood tests regularly”
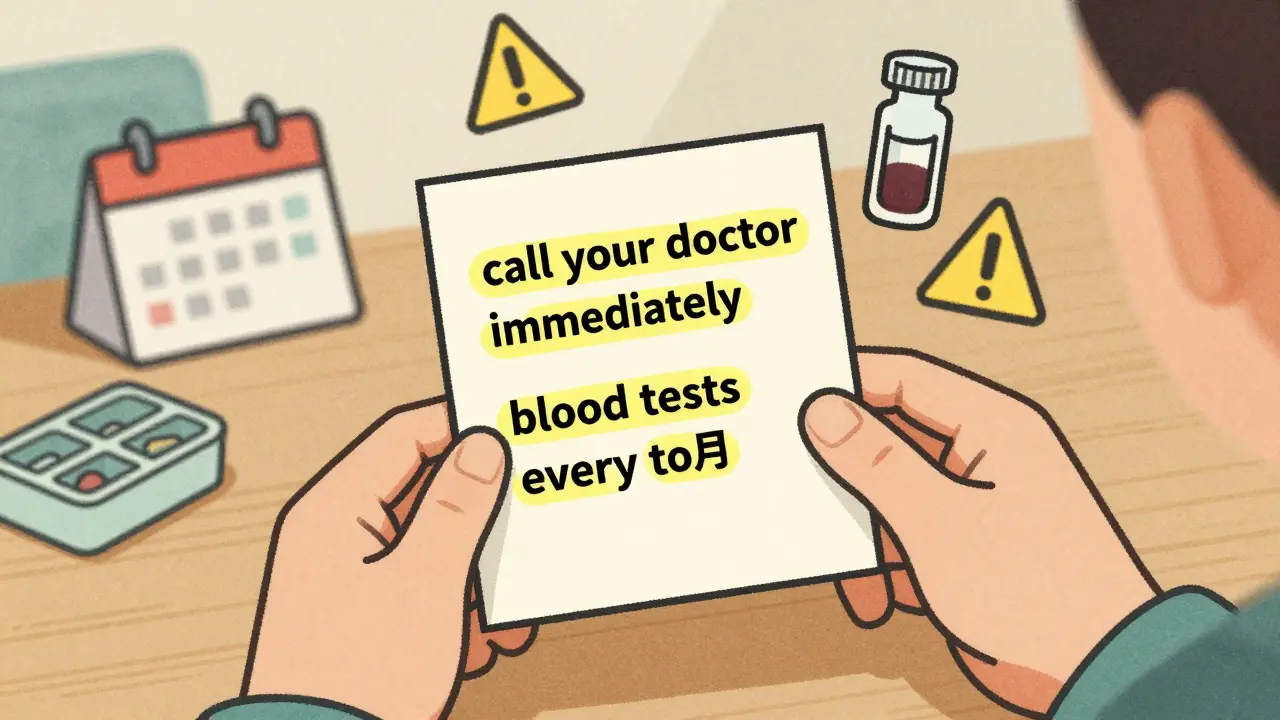
- “Call your doctor immediately if…”
- “Do not stop taking without talking to your doctor”
- “Avoid sunlight exposure”
- “Do not drink alcohol”
- “May impair driving ability”
- “Keep all scheduled appointments”
These aren’t just reminders. They’re triggers. If your guide says “get your blood tested regularly,” find out how often. Is it weekly? Monthly? Every three months? Write it down. Set a reminder on your phone. Miss one test, and you could be walking blind into a dangerous side effect.
Antidepressants like sertraline or venlafaxine all have the same warning: “Pay close attention to any changes, especially sudden changes, in mood, behavior, thoughts, or feelings.” That’s not vague. That’s a direct instruction to monitor yourself-and to tell someone if things feel off. The risk is highest in the first 4 to 6 weeks. That’s not a guess. That’s data from thousands of patients.
Numbers Tell the Real Story
Vague warnings like “may cause dizziness” don’t help. But when a guide says, “About 1 in 200 people taking clozapine may develop agranulocytosis,” that’s different. That’s a real number. That’s something you can weigh against your own risk.
Harvard Medical School found that when guides use exact percentages instead of vague terms, patient understanding improves by 47%. That’s huge. It means you’re more likely to notice a symptom early-and act on it.
Look for these kinds of numbers:
- “1 in 50 people may develop severe skin reactions”
- “15% of patients experience low white blood cell counts”
- “The risk of liver injury is 3 times higher in people over 65”
These aren’t scare tactics. They’re risk assessments. And they’re your best tool for deciding whether the benefits outweigh the dangers.
How to Actually Use This Information
Reading the guide is only half the battle. Using it is the other half.
Here’s what works:
- Use the 3-2-1 method. Spend 3 minutes reading the guide when you first get the prescription. Then, 2 minutes before each refill. And 1 minute every time you take the pill-just check if anything changed.
- Highlight and circle. Grab a yellow highlighter and mark every word like “test,” “monitor,” “check,” or “measure.” Circle every time frame: “weekly,” “monthly,” “after 2 weeks.” Underline anything that says “call your doctor immediately.”
- Create a monitoring calendar. If your guide says “blood tests every 3 months,” mark those dates on your phone calendar. Set a reminder 3 days before each one. Don’t wait for your doctor to remind you.
- Use the traffic light system. Green = normal. Yellow = watch this symptom, call your doctor. Red = go to the ER. Write these down on a sticky note and keep it with your pills.
- Keep a medication journal. Write down your test results, symptoms, and dates. Patients who did this had 68% fewer adverse events.
Pharmacist Sarah Chen in Bristol says she sees a huge difference when she takes just 90 seconds to point out the monitoring section: “Compliance with blood tests jumps from 45% to 82% when patients see exactly what to do.”
What If Your Guide Is Missing or Hard to Read?
By law, a medication guide must be given to you every time you fill your prescription. But in 2022, 41% of independent pharmacies didn’t consistently hand them out.
If you don’t get one:
- Ask for it. Say: “I need the FDA Medication Guide for this drug.”
- If they say no, call the pharmacy’s corporate office or file a complaint with the FDA.
- You can always download the official guide from DailyMed (a free NIH site). Just search your drug name and click “Patient Information.”
Some guides are still too long or too dense. That’s changing. Starting in 2026, the FDA will require pictograms-simple icons showing when to test, when to call, and what to watch for. But until then, you need to be the one to dig out the key details.
What’s Changing in 2026 and Beyond
Medication guides are evolving. By 2025, all drugs with Risk Evaluation and Mitigation Strategies (REMS) will need one. That’s 127 medications, up from 42. And starting in 2026, you’ll see QR codes on pill bottles that link directly to the latest guide.
Some companies are even testing AI-powered guides that personalize the information based on your age, health history, and other medications. Pfizer’s pilot showed a 63% improvement in how well patients understood their risks.
But here’s the catch: even with better design, 40% of U.S. adults still struggle with health literacy. That means if you’re reading this, you’re already ahead of the curve. You’re not waiting for someone else to explain it to you. You’re taking control.
Final Thought: This Is Your Health
Medication guides aren’t optional reading. They’re your last line of defense against preventable harm. A single missed blood test can turn a manageable side effect into a hospital visit. A misunderstood warning can lead to stopping your medicine too soon-or ignoring a symptom that should have been treated yesterday.
It doesn’t take hours. It doesn’t take a degree. It takes 5 minutes. Look for the red flags. Write down the dates. Know what to watch for. And never assume your doctor will catch it for you. They’re busy. You’re the one taking the pill. You’re the one who needs to know what it can do.

Lisa Rodriguez
I used to skip these guides till my cousin had a near-fatal reaction to an antibiotic because she didn't know about the liver warning. Now I read them like a detective. Highlight the red flags, write the test dates on my phone, and keep a sticky note with the traffic light system on my pill bottle. It's not rocket science but it saves lives.
Pro tip: If your pharmacy doesn't hand it to you, just ask for the FDA Medication Guide. They're legally required to give it. No excuses.